Everolimus for Advanced Breast Cancer: An Update From the BOLERO-2 Trial
The 18-month results of the phase III BOLERO-2 trial were presented at the ASCO Breast Cancer Symposium, confirming earlier survival results.
At the American Society of Clinical Oncology (ASCO) Breast Cancer Symposium last week, Hope Rugo, MD, director of breast oncology and clinical trials education and professor of medicine at the UCSF Helen Diller Family Comprehensive Cancer Center in San Francisco, presented the updated 18-month results of the BOLERO-2 trial.
Earlier results from the trial showed that everolimus combined with exemestane, an aromatase inhibitor, resulted in improved progression-free survival in women with previously treated, advanced estrogen-receptor–positive breast cancer.
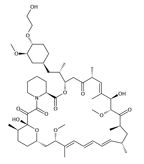
Chemical structure of everolimus
The BOLERO-2 trial compared everolimus, given at a dose of 10 mg per day in combination with the steroidal aromatase inhibitor exemestane at 25 mg per day to placebo plus exemestane. Patients were randomized two to one to either the experimental or the control arm, respectively.
The updated 18-month progression-free survival was 7.8 months for the everolimus arm compared to 3.2 months for the control arm of exemestane alone (hazard ratio = 0.45, P < .0001). These progression-free survival benefits were consistent for all subgroups analyzed, including age and geography. Patients with visceral metastases were a substantial portion of the overall trial and had a progression-free survival benefit comparable to the overall population.
Clinical benefit rates were double in the experimental group compared to the control group in the BOLERO-2 trial. “Response rate has been an allusive endpoint in second-line hormone therapy patients,” Dr. Rugo said during her presentation. Response rates were 1.7% in the exemestane-alone group compared to 12.6% in the everolimus group (P < .0001).
“This longer follow-up confirmed that the addition of everolimus to exemestane following progression on nonsteroidal aromatase inhibitors significantly improves progression-free survival, overall response rate, and response duration,” said Dr. Rugo.
Overall survival data continue to be promising and even more mature survival data are expected in 2013.
The US Food and Drug Administration (FDA) approved everolimus (Afinitor) based on the BOLERO-2 trial. The drug provides a new option for these previously treated patients who have limited treatment options otherwise. While many patients initially respond to aromatase inhibitors, all eventually relapse due to acquired resistance. Other current treatment options are other types of aromatase inhibitors as well as estrogen-receptor antagonists such as fulvestrant and tamoxifen.
“I use everolimus in combination with exemestane in patients whose disease has progressed or demonstrated resistance to a nonsteroidal aromatase inhibitor. I think that oncologists are now beginning to incorporate everolimus into this setting,” said Sara Hurvitz, MD, medical oncologist at the University of California in Los Angeles.
Everolimus is a phosphatidylinositol 3-kinase (PI3K)–Akt–mammalian target of rapamycin (mTOR) inhibitor. Upregulation of the PI3K-mTOR pathway has been found to be a mechanism of resistance to endocrine therapies for women with estrogen-positive breast cancer. Evidence for an interaction between the mTOR pathway and estrogen-receptor signaling has been shown.
Impetus for the large-scale BOLERO-2 trial came from results of two phase II trials-a neoadjuvant trial that showed a high response rate and a hormone-receptor–positive HER2-negative trial published in the Journal of Clinical Oncology.[1,2]
The 12-month results of the BOLERO-2 phase III trial (published in the New England Journal of Medicine in February), showed a median progression-free survival of 10.6 months for the experimental group compared to 4.1 months for the placebo group (P < .001). No overall survival results were reported at the time.
In a subanalysis of patients older than 65, the combination of everolimus plus exemestane improved progression-free survival in this patient population (hazard ration = 0.56). Elderly patients did not have more frequent high-grade adverse events compared with the general population.
“Overall, tolerance was fairly similar to the younger [patient] population-particularly in terms of risk of stomatitis,” said Dr. Rugo.
“The addition of everolimus to exemestane improved bone turnover and delayed progression specifically in bone,” said Dr. Rugo. As bone metastases are frequent in advanced breast cancer, the BOLERO-2 trial also analyzed differences in bone metastasis frequency, finding that disease progression in the bone was lower for the everolimus arm compared to the placebo arm, 3.03% vs 6.16%, respectively. This trend continued longer than 6 months. The authors conclude that everolimus is beneficial for deterring bone metastasis in this breast cancer patient population.
“I believe that the use of everolimus in combination with exemestane will become more common now that the drug is approved by the FDA, and as clinicians become more comfortable with using the drug and managing toxicity,” said Dr. Rugo, who added that if toxicity is well managed, the value of the improved progression-free survival can be substantial.
Everolimus is also being investigated for other breast cancer populations-advanced HER2-positive disease in combination with trastuzumab and chemotherapy, and for hormone-receptor positive disease, including as adjuvant and post-neoadjuvant treatment.
A major goal for investigators is to identify biomarkers that will predict which patients will respond to therapy with mTOR inhibitors and other agents that target the PI3K pathway. “Combinations of inhibitors of this and related pathways are under intense study,” Dr. Rugo emphasized.
References
1. Baselga, et al. Phase II Randomized Study of Neoadjuvant Everolimus Plus Letrozole Compared With Placebo Plus Letrozole in Patients With Estrogen Receptor–Positive Breast Cancer. J Clin Oncol. 2009;27:2630-2637.
2. Bachelot, et al. Randomized Phase II Trial of Everolimus in Combination With Tamoxifen in Patients With Hormone Receptor–Positive, Human Epidermal Growth Factor Receptor 2–Negative Metastatic Breast Cancer With Prior Exposure to Aromatase Inhibitors: A GINECO Study. J Clin Oncol. 2012;30: 2718-2724.