FDA Approves 18F-rhPSMA-7.3 to Identify Prostate Cancer in PET Imaging
18F-rhPSMA-7.3 injection is now available to help identify PSMA-positive lesions during PET imaging for patients with metastatic or recurrent prostate cancer.
The FDA has approved 18F-rhPSMA-7.3 injection to be used during PET scans to identify prostate-specific membrane antigens positive lesions for patients with prostate cancer.
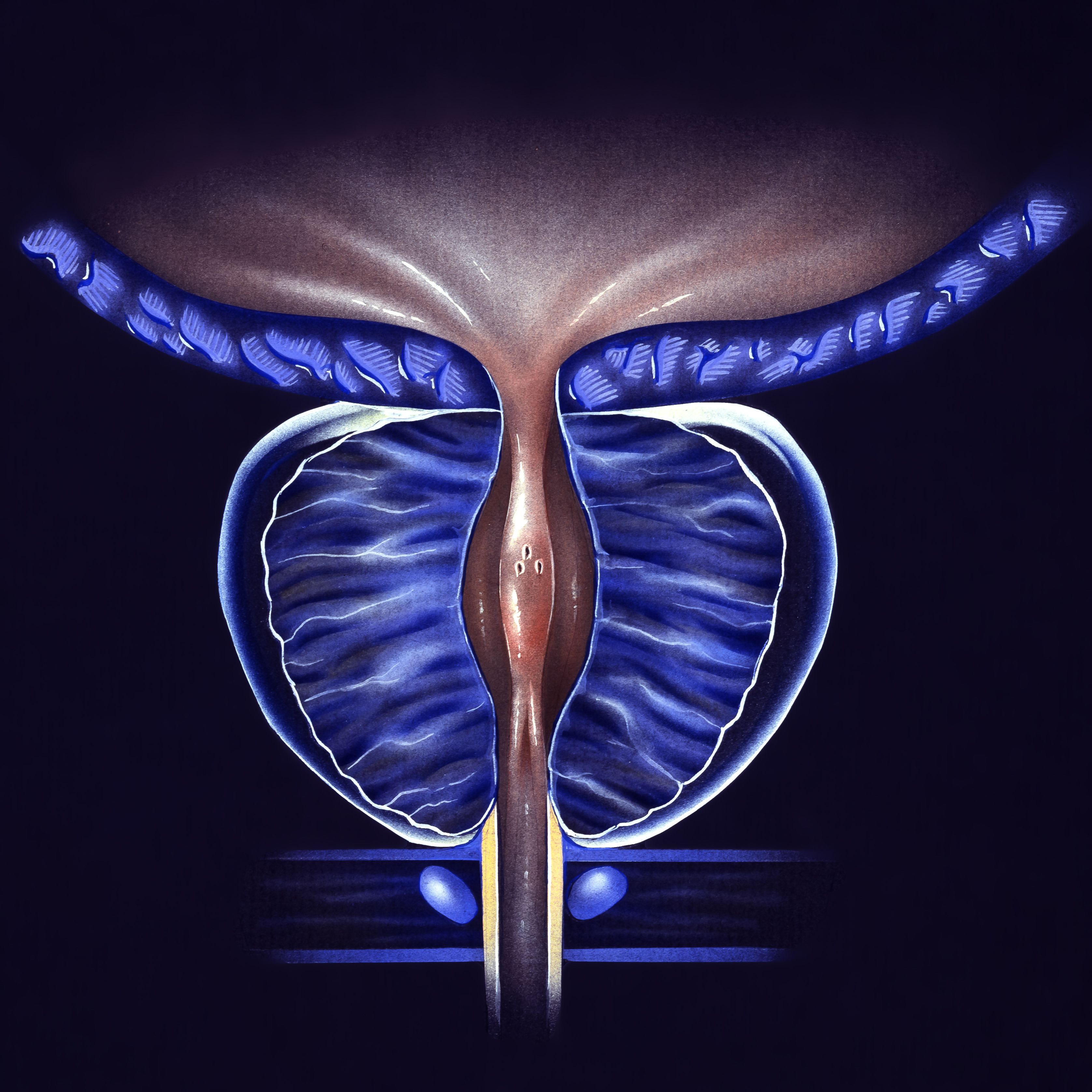
The FDA has approved 18F-rhPSMA-7.3 (Posluma) injection for use during PET scans to identify prostate-specific membrane antigen (PSMA)–positive lesions for patients with prostate cancer, according to a press release from Blue Earth Diagnostics.1
The approval is based on 2 phase 3 trials, LIGHTHOUSE (NCT04186819) and SPOTLIGHT (NCT04186845).2,3 Patients are eligible for this therapy if they have suspected metastases or recurrence based on prostate-specific antigen (PSA) levels.
18F-rhPSMA-7.3 was designed to advance PSMA-targeted molecules that bind to cells that express PSMA. Additionally, the 18F radioscope was designed to provide high-quality PET imaging and to determine where the disease is.
“Effective staging in newly diagnosed prostate cancer—determining its presence and helping determine whether it may have metastasized—is critical in establishing optimal clinical management strategies, because up to 25% of patients with primary prostate cancer may have detectable regional pelvic lymph node metastases, which are correlated with a risk for recurrence and associated overall survival,” Brian F. Chapin, MD, associate professor in the Department of Urology, Division of Surgery at The University of Texas MD Anderson Cancer Center, and coordinating investigator of the phase 3 LIGHTHOUSE study, said in the press release.
In the LIGHTHOUSE study, data was collected from 335 patients. These patients had a median PSA of 8.89 ng/mL, and between 16% to 28% had distant lesions detected by the 18F-rhPSMA-7.3 PET.
A patient level verified detection rate (VDR) was assessed by 3 readers. At the patient level, the VDR in reader 1 was 10% (95% CI, 7.4%-14.2%), 15% (95% CI, 11.0%-18.9%), and 11% (95% CI, 7.6%-14.6%) in reader 3. Across all 3 readers, investigators also evaluated extrapelvic lymph node VDR was 4.5% (95% CI, 2.5%-7.3%), 3.9% (95% CI, 2.1%-6.5%), and 3.6% (95% CI, 1.9%-6.2%); soft tissue parenchyma VDR was 1.8% (95% CI, 0.7%-3.9%) in all 3 readers; and bone VDR was 6.0% (95% CI, 3.7%-9.1%), 11.0% (95% CI, 7.6%-14.6%), and 7.2% (95% CI, 4.6%-10.5%).
A subgroup analysis of 314 patients was also conducted in those with negative conventional imaging at baseline. These data were similar to the overall population with the patient level of distant metastases VDR ranging between 9% to 13% across the readers.
The SPOTLIGHT study included 389 patients with a median PSA of 1.10 ng/mL, with the detection rates of the majority read of 83%. Patients were given 18F-rhPSMA-7.3 at a dose of 296 MBq and PET/CT scans were given between 50 to 70 minutes after injection. Additionally, biopsies were conducted within 60 days of the PET scan, and confirmatory imaging within 90 days.
For patients with baseline PSA levels of less than 0.5 ng/mL (n = 121), 0.5 to less than 1.0 ng/mL (n = 67), 1.0 to less than 2.0 ng/mL (n = 45), 2.0 to less than 5.0 ng/mL (n = 88), 5.0 to less than 10.0 ng/mL (n = 36), and 10.0 ng/mL or more (n = 32), the detection rate based on PSA levels were 64%, 76%, 93%, 98%, 94%, and 100%, respectively.
When safety was assessed, there were no serious adverse effects (AEs), however, 4.1% experienced at least 1 treatment-emergent AE related to 18F-rhPSMA-7.3. The most common AEs included hypertension (1.8%), diarrhea (1.0%), injection site reaction (0.5%), and headache (0.5%).
References
- U.S. FDA approves Blue Earth Diagnostics’ POSLUMA® (Flotufolastat F 18) injection, first radiohybrid PSMA-targeted PET imaging agent for prostate cancer. News release. Blue Earth Diagnostics. May 30, 2023. Accessed May 30, 2023. https://bit.ly/43baWPD
- Chapin BF, Koontz BF, LIGHTHOUSE Study Group. Detection of true positive M1 lesions by 18F-rhPSMA-7.3 PET in newly diagnosed prostate cancer: results from the phase 3 prospective LIGHTHOUSE study. J Clin Oncol. 2023;41(suppl 6):315. doi:10.1200/JCO.2023.41.6_suppl.315
- Lowentritt, B. Impact of Clinical Factors on 18F-rhPSMA-7.3 Detection rates in men with recurrent prostate cancer: findings from the phase 3 SPOTLIGHT study. Presented at 2022 American Society for Radiation Oncology Annual Meeting (ASTRO); October 23-26, 2022; San Antonio, TX. Abstract 1049. doi:10.1016j.ijrobp.2022.07.585
Prolaris in Practice: Guiding ADT Benefits, Clinical Application, and Expert Insights From ACRO 2025
April 15th 2025Steven E. Finkelstein, MD, DABR, FACRO discuses how Prolaris distinguishes itself from other genomic biomarker platforms by providing uniquely actionable clinical information that quantifies the absolute benefit of androgen deprivation therapy when added to radiation therapy, offering clinicians a more precise tool for personalizing prostate cancer treatment strategies.