FDA Expands VENTANA PD-L1 Assay Label for Cemiplimab in NSCLC Subtype
The VENTANA PD-L1 Assay becomes the only FDA-approved companion diagnostic with non–small cell lung cancer indications for 4 immunotherapy agents.
The FDA has approved an expanded label for the VENTANA PD-L1 (SP263) Assay as a companion diagnostic for identifying patients with locally advanced or metastatic non–small cell lung cancer (NSCLC) who may benefit from treatment with cemiplimab (Libtayo), according to a press release from Roche.1
The FDA previously approved cemiplimab plus chemotherapy for patients with advanced non–small cell lung cancer wihout EGFR, ALK, or ROS1 mutations in November 2022.
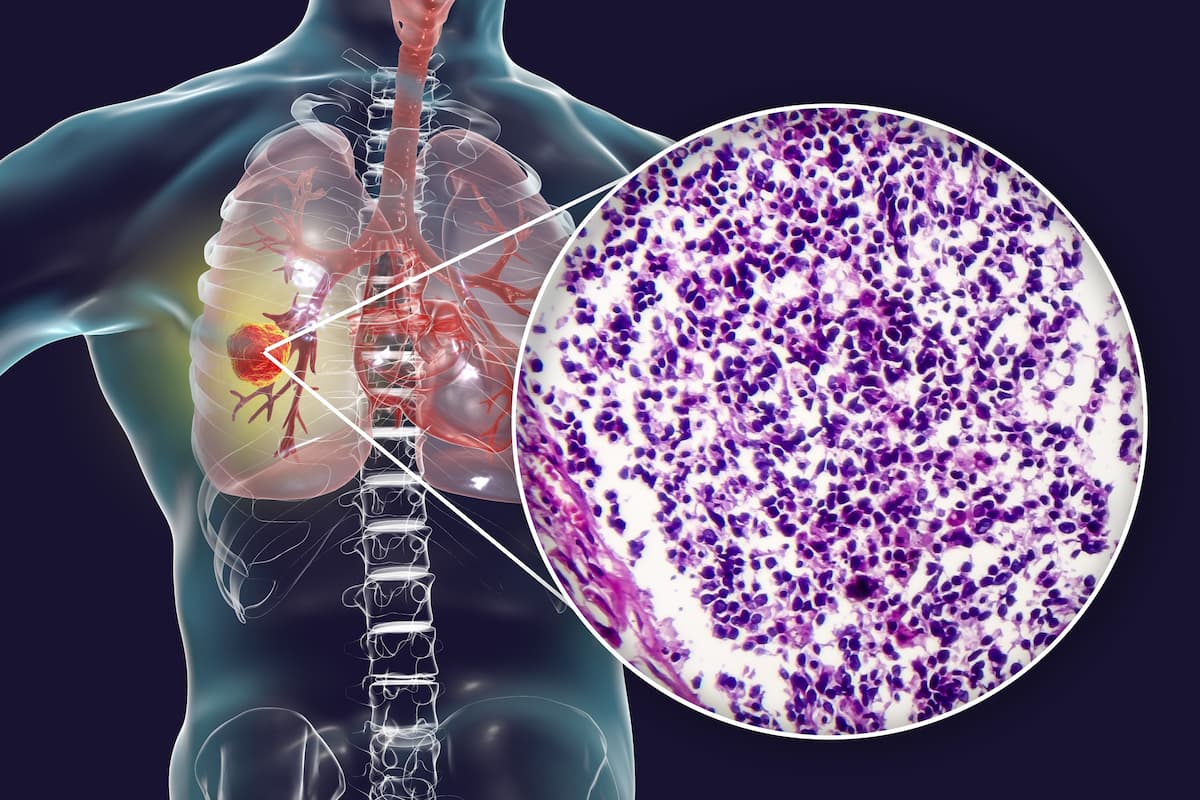
The VENTANA PD-L1 Assay was designed to detect PD-L1 proteins in NSCLC, which investigators have previously used in clinical studies to help predict the probability of patients benefitting from PD-1/PD-L1 immunotherapy agents including cemiplimab. Testing with the VENTANA PD-L1 Assay is performed with a BenchMark ULTRA instrument and is visualized with the OptiView DAB IHC Detection Kit.
“Diagnostics, like our high medical value PD-L1 assay portfolio, enable [personalized] medicine to help improve patient outcomes," Jill German, head of Pathology Lab at Roche Diagnostics, said in the press release. “This approval helps physicians make more confident treatment decisions by identifying patients with tumors that may respond to the immunotherapy [cemiplimab].”
The FDA previously approved cemiplimab plus chemotherapy for patients with advanced NSCLC without EGFR, ALK, or ROS1 mutations in November 2022.2 The approval was supported by data from the phase 3 EMPOWER-Lung 3 trial, (NCT03409614), in which investigators compared cemiplimab plus chemotherapy with placebo plus chemotherapy for patients with advanced NSCLC.
In the EMPOWER-Lung 3 trial, the median overall survival (OS) was 21.9 months (95% CI, 15.5-not evaluable [NE]) with the cemiplimab combination vs 13.0 months (95% CI, 11.9-16.1) with placebo (HR, 0.71; 95% CI, 0.53-0.93; P = .014).3
In patients with squamous histology, the median OS was 21.9 months (95% CI, 15.6-NE) vs 13.8 months (95% CI, 9.3-18.0) in each respective arm (HR, 0.56; 95% CI, 0.37-0.84). Among patients with nonsquamous disease, the median OS in each respective arm was 15.8 months (95% CI, 13.7-NE) vs 13.0 months (95% CI, 10.0-NE; HR, 0.79; 95% CI, 0.54-1.14).
Of 466 total patients, investigators randomly assigned 312 patients to the cemiplimab plus chemotherapy arm and 154 to the placebo plus chemotherapy arm.
The primary end point of the EMPOWER-Lung 3 trial was OS. Key secondary end points included progression-free survival, objective response rate, duration of response, best overall response, treatment-emergent adverse effects, and quality of life.
Patients 18 years and older with histologically or cytologically documented squamous or nonsquamous stage IIIB or IIIC NSCLC and PD-L1 expression in less than 50% of tumor cells as determined by an assay were eligible for enrollment on the trial. Additional inclusion criteria included having an availability archival or on-study formalin-fixed, paraffin-embedded tumor sample; at least 1 radiographically measurable lesion per RECIST v1.1 criteria; and a life expectancy of at least 3 months.
Previously, the FDA approved the VENTANA PD-L1 Assay as a companion diagnostic for determining which patients with NSCLC could be eligible to receive treatment with atezolizumab (Tecentriq) in October 2021.4 Investigators used the assay to identify PD-L1 expression in the phase 3 IMpower010 trial (NCT02486718).
References
- Roche receives FDA approval of label expansion for VENTANA PD-L1 (SP263) Assay to identify patients with locally advanced and metastatic non-small cell lung cancer eligible for Libtayo. News release. Roche. March 6, 2023. Accessed March 6, 2023. bit.ly/3yd49Ho
- FDA approves cemiplimab-rwlc in combination with platinum-based chemotherapy for non-small cell lung cancer. News release. FDA. November 8, 2022. Accessed March 6, 2023. https://bit.ly/3WO0BX1
- Gogishvili M, Melkadze T, Makharadze T, et al. Cemiplimab plus chemotherapy versus chemotherapy alone in non-small cell lung cancer: a randomized, controlled, double-blind phase 3 trial. Nat Med. Published online August 25, 2022. doi:10.1038/s41591-022-01977-y
- Roche’s VENTANA PD-L1 (SP263) assay receives FDA approval as a companion diagnostic to identify certain non-small cell lung cancer patients eligible for Tecentriq® (atezolizumab). News release. Roche. October 22, 2021. Accessed March 6, 2023. https://bit.ly/2ZbYL9L