FDA Grants Fast Track Designation for AC699 in ER+/HER2- Breast Cancer
Phase 1 AC699-001 results evaluating the safety and efficacy of AC699 in patients with breast cancer subtypes support the Fast Track designation.
Phase 1 AC699-001 results evaluating the safety and efficacy of AC699 in patients with breast cancer subtypes support the Fast Track designation.
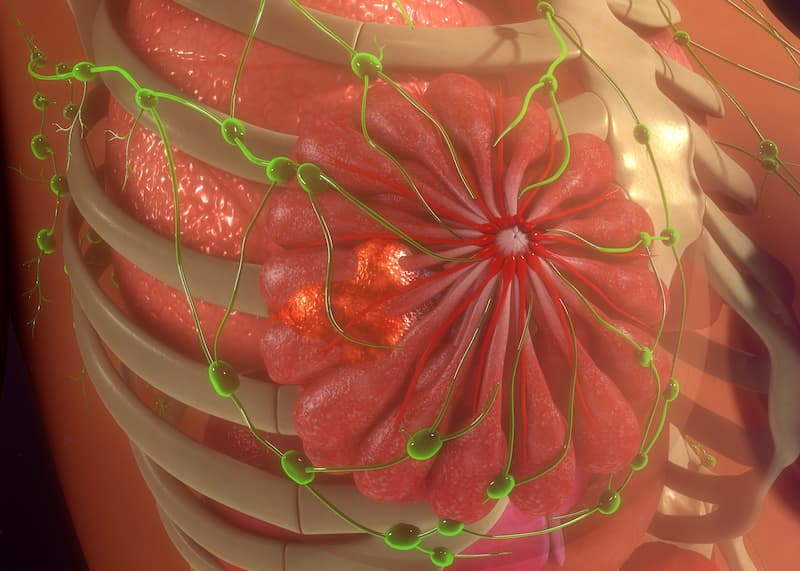
The FDA has granted Fast Track designation to AC699, an investigational chimeric degrader of estrogen receptor (ER), for the treatment in patients with ER-positive, HER2-negative, estrogen receptor 1 (ESR1)-mutated advanced or metastatic breast cancer with disease progression during or following at least 1 line of endocrine-based therapy, according to a news release published by the drug’s developer, Accutar Biotechnology Inc.1
The designation is supported by results from the phase 1 AC699-001 trial (NCT05654532) evaluating the safety, tolerability, pharmacokinetics, and preliminary antitumor activity of AC699 treatment in patients with ER-positive and HER2-negative locally advanced or metastatic breast cancer.2 Data show there were no dose-limiting toxicities, dose reductions, or discontinuations due to treatment-related AEs.
Additionally, among patients eligible for efficacy analysis, (n = 12), 4 (33%) achieved a partial response, including 3 of which were confirmed and 1 that was unconfirmed. Furthermore, the clinical benefit rate (CBR) was 42% (n = 5/12) among this patient group and included patients with stable disease for 24 or more weeks. In the patient subgroup with ESR1 mutations (n = 6), the overall response rate (ORR) was 67% (n = 4/6) and the CBR was 83% (n = 5/6) for a median treatment time of 168 days (range, 56-336).
"Receiving Fast Track designation for AC699 from the FDA highlights their recognition of the serious and life-threatening nature of this malignancy, the critical unmet medical needs not fully addressed by existing therapies, and the potential of AC699 to fill in the gap," Jie Fan, PhD, chief executive officer of Accutar Biotechnology, Inc, stated in the news release.1 "We look forward to working closely with the FDA to optimize and expedite the development program."
The phase 1 study employed a 3+3 design, with the possibility of adding backfill to patients each cleared cohort deemed safe. In total, 22 patients with locally advanced or metastatic ER-positive/HER2-negative breast cancer having received at least 2 prior lines of endocrine treatment or at least 1 combined with a CDK4/6 inhibitor received AC699 treatment. Prior treatments include CDK4/6 inhibitor (100%), aromatase inhibitor (91%), fulvestrant (Faslodex; 82%), novel oral SERD or covalent antagonist (23%), and an ER chimeric degrader (14%).
By the data cutoff date, 3 dose cohorts were established at 100 mg, 200 mg, and 300 mg. Patients received oral AC699 once daily in 28-day cycles. Of the 22 patients having received AC699 therapy, only 15 had scans prior to data cutoff; of the 15 patients, 3 were not evaluable for efficacy analysis due to having only bone lesions.
Tumor responses were assessed every 2 cycles using RECIST 1.1 criteria. An exploratory analysis investigated the relationship between antitumor activity and ESR1 mutational status.
Coprimary endpoints include dose-limiting toxicities and treatment-emergent adverse events (TEAEs).3 Key secondary end points include ORR, CBR, duration of response (DOR), disease control rate, progression-free survival, and pharmacokinetics.
Common TEAEs included fatigue (23%), dehydration (18%), and nausea (18%). Treatment-related AEs were grade 2 or lower and included nausea (18%) and hot flushes (14%). As of the cutoff date, 4 patients were still receiving AC699 therapy.
Additional inclusion criteria include adult patients with a life expectancy of 12 or more weeks after the start of treatment, acceptable organ and hematologic function, and at least 1 measurable lesion according to RECIST or at least 1 predominately lytic bone lesion in the absence of measurable disease.
“Preliminary data from the ongoing phase 1 trial evaluating AC699 indicate promising safety, tolerability, and anti-tumor activity, at doses up to 300 mg orally once daily. A phase 2 study will begin enrolling in early 2024,” Manish R. Patel, MD, medical oncologist and director of drug development at the Sarah Cannon Research Institute, concluded in the study abstract presented at the 2024 ASCO Annual Meeting.2
References
- Accutar Biotechnology receives FDA Fast Track designation for AC699 in ER+ / HER2- breast cancer. News release. Accutar Biotechnology Inc. August 14, 2024. Accessed August 15, 2024. https://tinyurl.com/4rvhmxde
- Patel MR, Layman RM, Danso MA, et al. Preliminary results from a phase 1 study of AC699, an orally bioavailable chimeric estrogen receptor degrader, in patients with advanced or metastatic breast cancer. J Clin Oncol. 2024;42(suppl 16). doi:10.1200/JCO.2024.42.16_suppl.3074
- Study of AC699 in patients with estrogen receptor positive/human epidermal growth factor receptor 2 negative (ER+/HER2-) locally advanced or metastatic breast cancer. ClinicalTrials.gov. Updated February 7, 2024. Accessed August 15, 2024. https://clinicaltrials.gov/study/NCT05654532