FDA Grants Orphan Drug Designation to GPRC5D Target in Multiple Myeloma
SAR446523 is currently being evaluated in a first-in-human phase 1 trial in patients with pretreated relapsed/refractory multiple myeloma.
SAR446523 is currently being evaluated in a first-in-human phase 1 trial in patients with pretreated relapsed/refractory multiple myeloma.
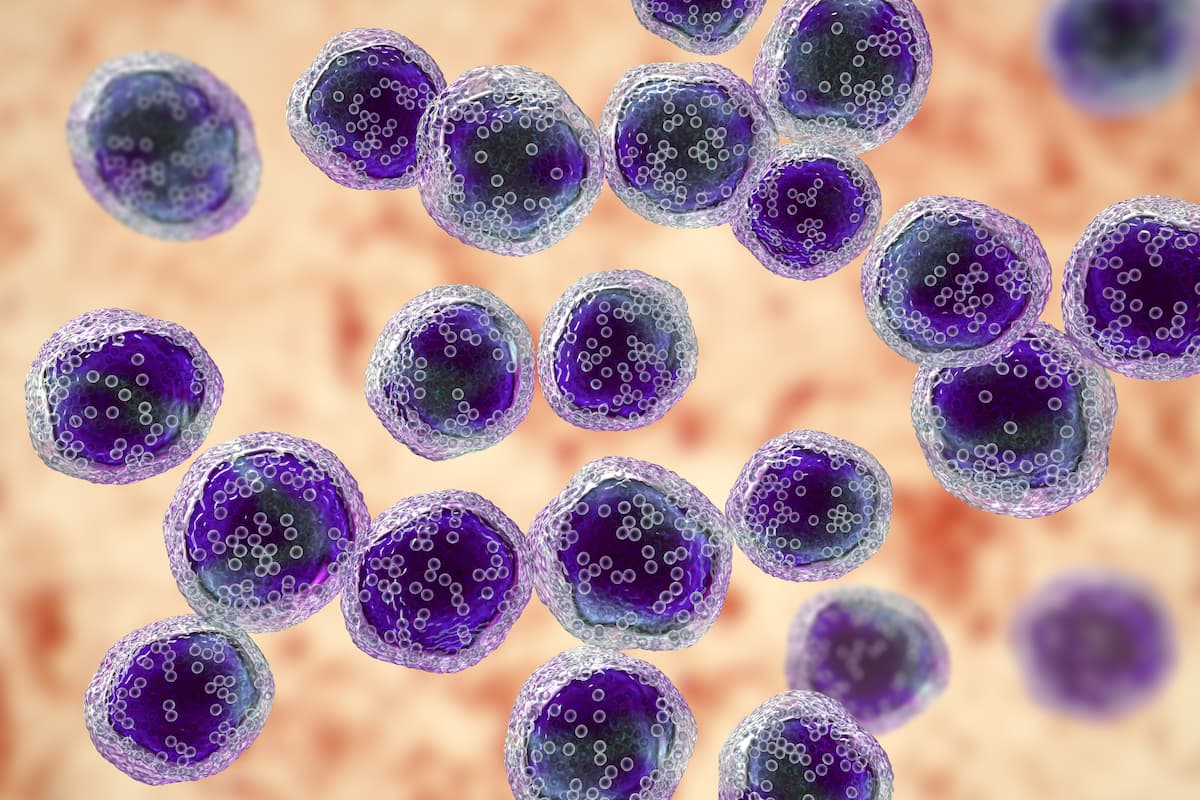
The FDA has granted orphan drug designation to SAR446523 for the treatment of patients with relapsed/refractory multiple myeloma, according to a press release from the developer, Sanofi.1 SAR446523 is an IgG1-based, antibody-dependent cellular cytotoxicity–enhanced monoclonal antibody targeting GPRC5D.
The agent targets GPRC5D via an engineered fragment crystallizable domain so that it enhances antibody-dependent cell-mediated cytotoxicity.
No regulatory authority has evaluated the safety and efficacy of SAR446523, and the agent remains under investigation.
The safety, antitumor activity, pharmacokinetics, and pharmacodynamics of subcutaneous SAR446523 in patients with relapsed/refractory multiple myeloma are currently being evaluated in the first-in-human, open-label phase 1 TED18162 trial (NCT06630806).2
“The orphan drug designation is a significant milestone in our ongoing efforts to develop innovative treatments in multiple myeloma,” Alyssa Johnsen, MD, PhD, global therapeutic area head of immunology and oncology development at Sanofi, said in the press release.1 “This underscores our commitment to multiple myeloma, a disease for which we have acquired strong expertise with the development of another widely used and approved immunotherapy treatment.”
The trial was initiated on October 30, 2024, and has an estimated completion date of May 14, 2029. There are 2 parts to this study: part A, the dose-escalation phase, which will analyze up to 6 dose levels of SAR446523 to identify the maximum administered dose, maximum tolerated dose, and recommended dose range of the 2 doses that will be evaluated in the second part, and part B, the dose-optimization phase, which will randomly assign patients 1:1 to one of the 2 dosing regimens identified in part A to find the recommended phase 2 dose.
Subcutaneous SAR446523 administration will be done at 6 dose levels; all patients will receive the agent once weekly for cycle 1 and then once every other week for every subsequent cycle, with a cycle length of 28 days.3
The estimated trial enrollment is 82 patients. Those who are eligible will be 18 years or older with a documented diagnosis of multiple myeloma and with measurable disease who use contraceptives consistent with local regulations. In part A, patients are required to have received at least 3 prior lines of antimyeloma therapy for which they have experienced relapse or have been refractory or intolerant to; prior exposure to anti-GPRC5D therapy and anti-BCMA therapy is permitted. In part B, patients are required to have received at least 3 prior lines of antimyeloma therapy and have experienced relapse from or been refractory to an immunomodulatory agent, a proteasome inhibitor, an anti-CD38 monoclonal antibody, and an anti-BCMA targeting agent; prior exposure to anti-GPRC5D therapy is not allowed.
Reasons for trial exclusion include an ECOG performance status of 2 or higher; receipt of systemic antimyeloma treatment within 14 days before first study treatment administration; prior treatment with natural killer cell–engaging therapy within 90 days of study treatment; primary systemic and localized amyloid light chain amyloidosis, active polyneuropathy, organomegaly, endocrinopathy, myeloma protein, skin changes syndrome, and active plasma cell leukemia; inadequate organ and marrow function; and significant concomitant illness.
The trial’s primary end point in part A is the incidence of dose-limiting toxicities, and in part B, the primary end point is the overall response rate. Secondary end points include the number of patients with treatment-emergent adverse events, the change from baseline in laboratory abnormalities, the very good partial response or better rate, the clinical benefit rate, the duration of response, the time to response, the progression-free survival, the minimal residual disease negativity, and the number of patients with symptomatic adverse events.
References
- Press release: Sanofi’s SAR446523, a GPRC5D monoclonal antibody, earns orphan drug designation in the US for multiple myeloma. News release. Sanofi. July 30, 2025. Accessed July 30, 2025. https://tinyurl.com/3e5p9z8x
- A study to investigate the safety and efficacy of SAR446523 injected subcutaneously in adult participants with relapsed/refractory myeloma. ClincialTrials.gov. Updated April 23, 2025. Accessed July 30, 2025. https://tinyurl.com/3nz922ye
- Kapoor P, Ailawadhi S, Pavic M, et al. First-in-human, open-label, phase 1 trial design of SAR446523, a novel anti-GPRC5D antibody-dependent cellular cytotoxicity (ADCC)-enhanced monoclonal antibody for multiple myeloma. Abstract presented at: European Hematology Association 2025 Congress; June 12-15, 2025; Milan, Italy. Abstract PB2983.
Navigating AE Management for Cellular Therapy Across Hematologic Cancers
A panel of clinical pharmacists discussed strategies for mitigating toxicities across different multiple myeloma, lymphoma, and leukemia populations.