FDA Issues Refusal to File Letter for Nogapendekin Alfa Inbakicept in NMIBC
The FDA refuses to file the sBLA for nogapendekin alfa inbakicept plus BCG in BCG-unresponsive NMIBC with papillary disease without carcinoma in situ.
The FDA refuses to file the sBLA for nogapendekin alfa inbakicept plus BCG in BCG-unresponsive NMIBC with papillary disease without carcinoma in situ.
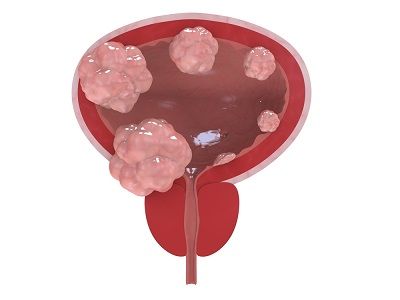
The FDA sent a refusal to file (RTF) letter to ImmunityBio regarding the supplemental biologics license application (sBLA) submitted in April 2025 for nogapendekin alfa inbakicept-pmln (Anktiva) in combination with BCG in the treatment of BCG-unresponsive non–muscle-invasive bladder cancer (NMIBC) with papillary disease without carcinoma in situ (CIS), according to a press release from the developer, ImmunityBio.1,2
The RTF letter was received on May 2, 2025, and has been deemed “inconsistent” by the developer. The letter only affects patients with papillary disease without CIS; the letter does not affect the prior approval of the treatment in patients with BCG-unresponsive NMIBC with papillary disease with CIS.3
The developer claimed that leadership of the FDA gave unanimous guidance and encouragement to submit the sBLA at an in-person meeting in January 2025; the FDA’s Center for Biologics Evaluation and Research, Center for Drug Evaluation and Research, and Oncology Center of Excellence were all part of the meeting and similarly encouraged the submission of the sBLA.
An urgent meeting has already been requested by the developer to “resolve the inconsistencies between the directives provided at the January meeting and receipt of the RTF letter.”1
“We are fully determined to work with the FDA as quickly as possible, including having already requested a Type A meeting, to explore the best path forward. We would also welcome an FDA advisory committee meeting as part of the regulatory process going forward,” said Patrick Soon-Shiong, MD, founder, executive chairman, and global chief scientific and medical officer at ImmunityBio, in the press release.1 “We presented our data at the recent 2025 American Urological Association meeting, and [nogapendekin alfa inbakicept plus] BCG was considered best in class and best in disease by the thought leaders in attendance when compared with all the therapies currently approved or in development.”
Results supporting nogapendekin alfa inbakicept came from the single-arm, open-label, phase 2/3 QUILT-3.032 trial (NCT03022825), which evaluated the agent in combination with BCG in patients with BCG-unresponsive NMIBC.
At 36 months, more than 82% of patients with papillary disease without CIS and 84% of patients with papillary disease and CIS had cystectomy avoidance. In patients without CIS and patients with CIS, disease-specific survival was 99% and 100%, respectively, at 12 months, and 96% and 99%, respectively, at 36 months.
Additionally, the median disease-free survival among those without CIS was 19.3 months (95% CI, 7.4-not reached).4 The progression-free survival rate at 12 months was 97.1% (95% CI, 88.8%-99.3%); at 18 months, it was 94.8% (95% CI, 84.3%-98.3%); and at 24 months, it was 88.8% (95% CI, 74.1%-95.4%). The overall survival rate at 12 months was 98.6% (95% CI, 90.2%-99.8%); at 18 months, it was 94.3% (95% CI, 82.9%-98.1%); and at 24 months, it was 91.7% (95% CI, 79.0%-96.9%).
Rachel Sherman, MD, MPH, the former FDA principal deputy commissioner, added in the press release, “I actively participated in the January 2025 meeting at which the leadership of the agency present at that meeting unanimously supported and encouraged ImmunityBio to submit results from the single-arm trial, QUILT 3.032, as an sBLA because of the high risk of progression and metastasis these patients with BCG unresponsiveness [have]. The consensus was reached by all present, including me, because of the lack of satisfactory alternatives in this desperately ill population at high risk of losing their bladder—a life-threatening and life-changing procedure.”
Sherman also added, “Furthermore, it is incomprehensible to me that the FDA refuses to file an [sBLA], stating the study is not sufficient to support a regulatory review, when it has already approved a product based on that very same study in essentially the same indication and population…. These patients [have] a disease with a high risk of morbidity and mortality in the very short term; no delay should be tolerated.”
Cohort B, the cohort of patients with papillary disease without CIS, included a total of 80 patients. All patients in the cohort received nogapendekin alfa inbakicept plus BCG via a urinary catheter for 6 consecutive weeks in the initial induction treatment period.5 After the first assessment, patients received either a 3-week maintenance course or a 6-week reinduction course at month 3. Those who were eligible received maintenance treatment at months 6, 9, 12, and 18, and those who were eligible had the option to receive maintenance treatment at months 24, 30, and 36.
Eligible patients in the trial were 18 years or older with histologic confirmation of NMIBC of the transitional cell carcinoma high-grade subtype and histologic confirmation of presence of BCG-unresponsive CIS or BCG-unresponsive high-grade Ta or T1 disease.5 BCG-unresponsive disease was defined as persistent or recurrent CIS with or without Ta/T1 disease within 12 months of receiving adequate BCG, recurrent high-grade Ta/T1 disease within 6 months of completing adequate BCG, or T1 high-grade disease at first evaluation following induction BCG alone.
Cohort B’s primary end point was the disease-free rate at 12 months. Secondary end points included disease-free survival, disease-specific survival, time to cystectomy, and safety.
In cohorts A and B combined, 86% of patients experienced at least 1 treatment-emergent adverse event (TEAE) of grade 1 or 2; of grade 3 TEAEs, 20% experienced at least 1.4 The most common grade 1/2 TEAEs were dysuria (30%), pollakiuria (25%), and hematuria (25%).
“The agency must explain the confounding inconsistency of approving [nogapendekin alfa inbakicept plus] BCG for patients with papillary with CIS disease while refusing to file the sBLA for patients with papillary without CIS disease—even though both groups were part of the same trial, in the same high-risk population of BCG-unresponsive [NMIBC],” Soon-Shiong concluded.1 “On behalf of patients facing a potential loss of a vital organ and high risk of progression of disease, I urge the agency to reconsider and act now.”
References
- ImmunityBio requests an urgent meeting with FDA to address the change in the agency’s unambiguous guidance on Jan 2025 to submit a sBLA for NMIBC BCG unresponsive papillary disease, following an inconsistent refusal to file letter on May 2, 2025. News release. ImmunityBio. May 5, 2025. Accessed May 5, 2025. https://tinyurl.com/mrxe54vp
- ImmunityBio announces FDA submissions of supplemental BLA for NMIBC papillary disease and for expanded access of ANKTIVA to treat lymphopenia. News release. ImmunityBio. April 15, 2025. Accessed May 5, 2025. https://tinyurl.com/4atzxwjv
- FDA approves nogapendekin alfa inbakicept-pmln for BCG-unresponsive non-muscle invasive bladder cancer. FDA. April 22, 2024. Accessed May 5, 2025. https://tinyurl.com/b8d9672c
- Chamie K, Chang SS, Kramolowsky E, et al. IL-15 superagonist NAI in BCG-unresponsive non–muscle-invasive bladder cancer. N Engl J Med Evid. 2023;2(1). doi:10.1056/EVIDoa2200167
- QUILT-3.032: a multicenter clinical trial of intravesical Bacillus Calmette-Guerin (BCG) in combination with ALT-803 (N-803) in patients with BCG unresponsive high grade non-muscle invasive bladder cancer. ClinicalTrials.gov. Updated April 13, 2025. Accessed May 5, 2025. https://tinyurl.com/5a5vetsz