FDA Requests Withdrawal of Ibrutinib in US for Lymphoma Indications
Primary outcome data from phase 3 confirmatory studies evaluating ibrutinib in mantle cell lymphoma and marginal zone lymphoma are insufficient to support conversion to full FDA approval in these indications.
Intent to voluntarily withdraw indications for the accelerated approval of ibrutinib (Imbruvica) in previously treated mantle cell lymphoma (MCL) and marginal zone lymphoma (MZL) following consultation with the FDA, has been indicated by the manufacturers of the treatment, according to a press release from Johnson & Johnson and Pharmacyclics.1
"While withdrawing these indications was a difficult decision, we remain confident in the benefit/risk profile of [ibrutinib] in its approved indications and are committed to its continued development,” according to the manufacturers of ibrutinib.
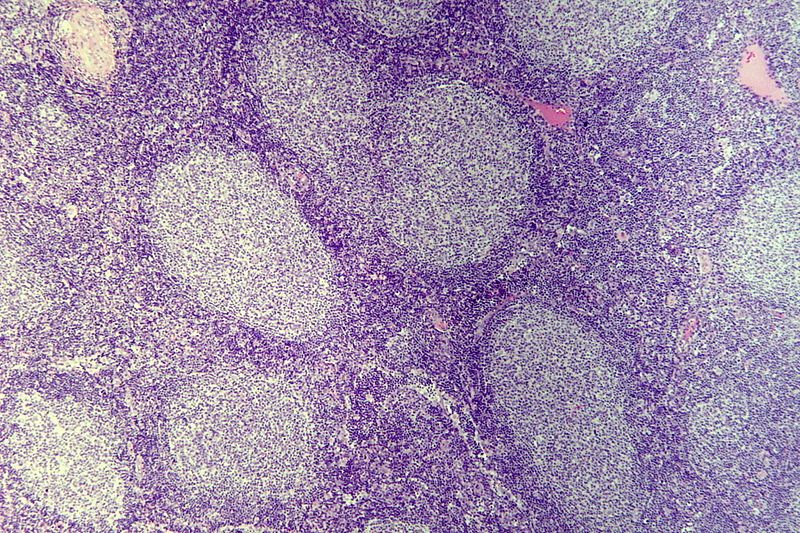
Accelerated approval of ibrutinib in these indications was based on the overall response rate (ORR) in 2 phase 2 trials. The demonstration of clinical benefit in the phase 3 SHINE study (NCT01776840) in patients with previously untreated MCL and the phase 3 SELENE study (NCT01974440) in those with relapsed/refractory MZL or follicular lymphoma. Following a discussion with the study investigators, the FDA stated that primary end point data from these trials were insufficient to support a full approval of ibrutinib.
According to data from the phase 3 SHINE study presented at the 2022 American Society of Clinical Oncology (ASCO) Annual Meeting, ibrutinib met the primary end point of progression-free survival (PFS).2 Additionally, findings published in The New England Journal of Medicine highlighted that the median PFS was 80.6 months (95% CI, 61.9-not evaluable) in the ibrutinib-based arm vs 52.9 months (95% CI, 43.7-71.0) in the placebo arm (stratified hazard ratio [HR], 0.75; 95% CI, 0.59-0.96; P = .01).3 However, overall survival (OS) was similar in the 2 treatment groups (HR, 1.07; 95% CI, 0.81-1.40).
In the phase 3 SELENE study, ibrutinib did not reach the primary end point of PFS in those with follicular lymphoma or MZL. Investigators will present study results at a later scientific forum.
“While withdrawing these indications was a difficult decision, we remain confident in the benefit/risk profile of [ibrutinib] in its approved indications and are committed to its continued development,” Craig Tendler, MD, vice president of Late Development and Global Medical Affairs at Janssen Research & Development, LLC, said in the press release.
Investigators of the randomized, double-blind, placebo-controlled phase 3 SHINE study assessed ibrutinib in combination with bendamustine plus rituximab (Rituxan) in patients with newly diagnosed MCL. Patients were randomly assigned to receive 90 mg/m2 of bendamustine intravenously on days 1 and 2 of cycles 1 to 6, 375 mg/m2 of rituximab intravenously on day 1 of cycles 1 to 6, and 560 mg of ibrutinib capsules or matched placebo orally once a day until disease progression or unacceptable toxicity.
Secondary end points of the SHINE study included OS, complete response (CR) rate, time-to-next treatment, ORR, and duration of response (DOR).
Patients 65 years and older with clinical stage II, III, or IV MCL by Ann Arbor classification were eligible to enroll in the SHINE study. Additional inclusion criteria included having at least 1 measurable site of disease, no prior therapies for MCL, and an ECOG performance status of 0 or 1.
Investigators of the phase 3 SELENE study evaluated ibrutinib in combination with bendamustine plus rituximab or rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) in patients with previously treated indolent non-Hodgkin lymphoma. Patients were randomly assigned to receive 560 mg of ibrutinib orally once daily, or 4 140 mg capsules, or matched placebo in combination with bendamustine plus rituximab or the R-CHOP regimen.
Secondary end points of the SELENE study included OS, CR rate, ORR, and DOR.
Patients 18 years and older with a histologically confirmed diagnosis of follicular lymphoma or MZL and at least 1 prior treatment with a regimen including a CD20 antibody were eligible for enrollment in the SELENE study. Additional inclusion criteria included having relapsed or refractory disease, at least 1 measurable site of disease, and an ECOG performance status of 0 or 1.
References
- Update on IMBRUVICA® (ibrutinib) U.S. accelerated approvals for mantle cell lymphoma and marginal zone lymphoma indications. News release. Johnson & Johnson and Pharmacyclics. April 6, 2023. Accessed April 10, 2023. bit.ly/3ZUpDnJ
- Wang ML, Jurczak W, Jerkeman M et al. Primary results from the double-blind, placebo-controlled, phase III SHINE study of ibrutinib in combination with bendamustine-rituximab (BR) and R maintenance as a first-line treatment for older patients with mantle cell lymphoma (MCL). J Clin Oncol. 2022; 40(suppl_17):LBA7502. doi:10.1200/JCO.2022.40.17_suppl.LBA7502
- Wang ML, Jurczak W, Jerkeman M, et al. Ibrutinib plus bendamustine and rituximab in untreated mantle-cell lymphoma. N Engl J Med. 2022;386(26):2482-2494. doi:10.1056/NEJMoa2201817
Highlighting Insights From the Marginal Zone Lymphoma Workshop
Clinicians outline the significance of the MZL Workshop, where a gathering of international experts in the field discussed updates in the disease state.