From Increased Risks to Care Barriers: Experts Highlight Unique Challenges of LGBTQ+ Cancer Community
Key leaders in the oncology space discuss unique cancer risk factors, barriers to care, and ways in which institutions and organizations are creating more welcoming environments for individuals within the LGBTQ+ community.
Although conversations surrounding disparities among patients with cancer within the lesbian, gay, bisexual, transgender, queer/questioning, and plus (LGBTQ+) community have become more prevalent in recent years, a litany of barriers to care remain.
To ensure these barriers are appropriately addressed, one expert argued that questions about a patient’s sexual orientation and gender identity must become common practice to better educate patients about their risks.
Assessing Risk Factors Associated with Cancer for Transgender Vs Cisgender People
Of note, themes surrounding equity and inclusion in LGBTQ+ populations with cancer were prevalent at the recent 2022 American Society of Clinical Oncology (ASCO) Annual Meeting. For example, one real-world data analysis from a tertiary health care institution assessed cancer risk factors and disease incidence among transgender individuals compared with cisgender individuals.1
“There’s a lot that we don’t know about transgender people with cancer, and part of the reason is that we don’t routinely and systematically collect gender identity information within clinical settings or large population-based surveys. There is a national movement in the United States to [start collecting] sexual orientation and gender identity data in a more systematic and continuous way so that we can have more data,” lead investigator Ash B. Alpert, MD, MFA, a post-doctoral fellow in health services research at the Center for Gerontology and Healthcare Research in the Department of Health Services, Policy, & Practice at Brown University School of Public Health, said in an interview with CancerNetwork®.
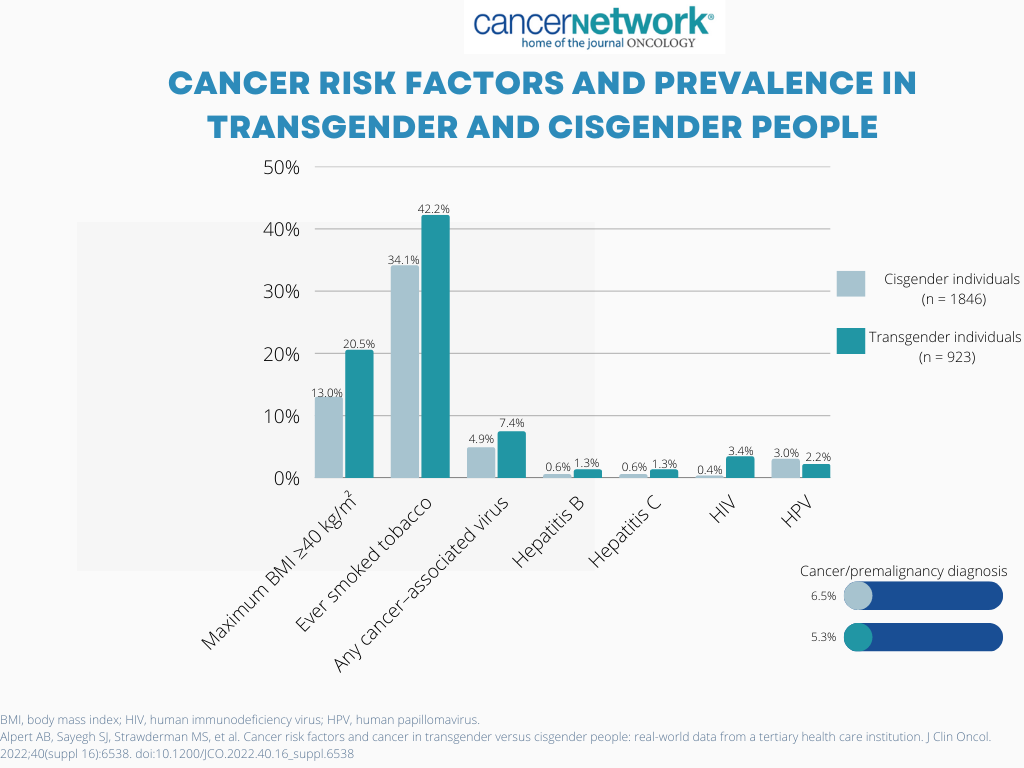
To conduct the research, investigators used a combination of structured gender identity data, diagnosis codes, and keyword searches to identify transgender patients within the tertiary care facility. The cisgender cohort was identified and matched based on age, first year of encounter, and years of follow-up. The analysis included a population of 923 transgender patients and 1846 cisgender patients. According to Alpert, higher rates of smoking (42% vs 34%; P <.0001), body mass index (BMI) of 40 or more (21% vs 13%; P <.0001), and human immunodeficiency virus (HIV; 3% vs 0%; P <.0001) were observed in transgender vs cisgender individuals.
“There are more people living with HIV who are transgender than [those] who are cisgender. We know that in the United States, approximately 40% of Black transgender people are living with HIV,” they said. “The data about smoking are very mixed. It really depends what study you’re looking at. The US Transgender Survey, which is one of the largest surveys of transgender people in the US, did not find a significant difference in smoking prevalence between transgender and cisgender people.”2
Table1. Cancer Risk Factors and Prevalence in Transgender and Cisgender People
Cancer risk factors in transgender individuals is an area that has primarily remained unexamined within the oncology space, Alpert explained. In particular, they noted that the association between interpersonal violence and cancer risk factors within the transgender community needs to be further examined by oncology at large.3 Investigators theorized that the high rate of interpersonal violence within the transgender community could increase the risk of cancer due to their direct effect on other cancer-related risk factors.
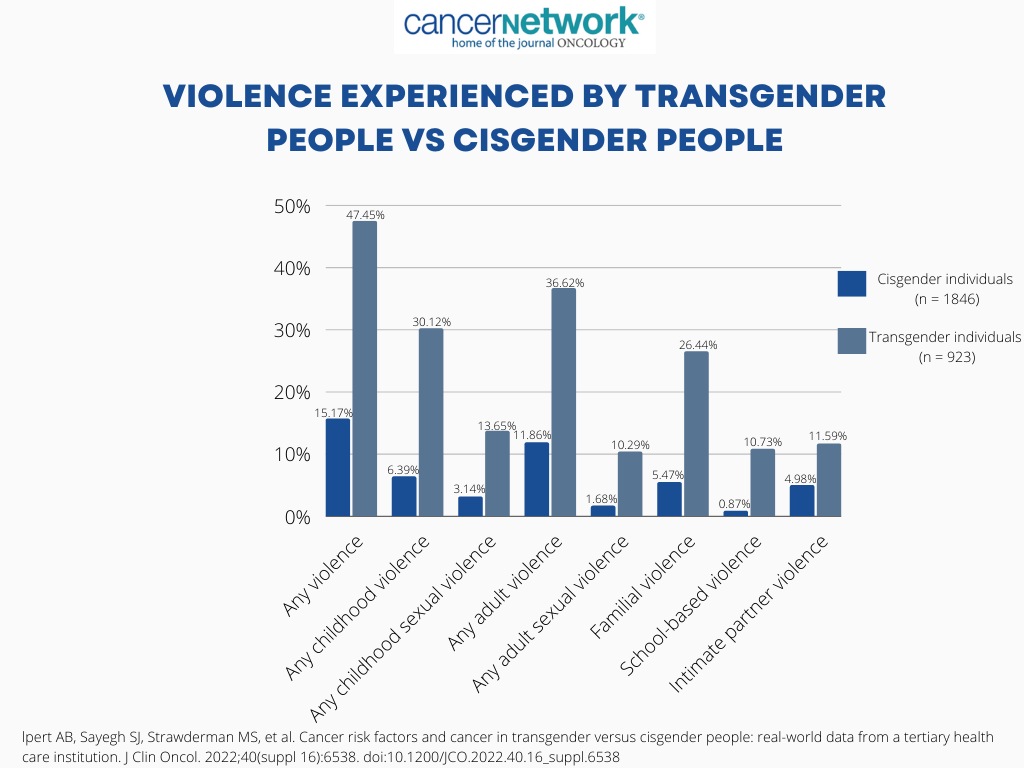
To further assess this, investigators identified 923 transgender patients and 1846 cisgender patients who were matched by age and follow-up time. The investigators then assessed for experiences of violence in both cohorts. From there, it was determined whether there was an association between those experiences and cancer risk factors, such as smoking and a BMI of 40 or more. Compared with cisgender individuals, transgender persons were more likely to encounter violence overall (47.45% vs 15.17%, respectively) as well as childhood (30.12% vs 6.39%) and familial violence (26.44% vs 5.47%).4
Table2. Violence Experienced by Transgender People Vs Cisgender People
Transgender individuals who experienced violence overall compared with those who didn’t were significantly more likely to be smokers (50% vs 35%, respectively; P <.0001) and have a BMI of 40 or more (23% vs 18%; P = .05). Similar associations were identified in the cisgender population, with those who experienced violence being significantly more likely to smoke (52%) and have a higher BMI (23%) than those who didn’t experience violence (31%; P <.0001; 11%; P <.001, respectively).
No statistically significant difference was demonstrated in terms of the association between violence and smoking in the transgender cohort vs the cisgender cohort (prevalence ratio [PR], 0.87; P = .17). However, a statistically significant difference was observed when assessing the association between violence and higher BMI in transgender individuals vs cisgender individuals. (PR, 0.65; P = .02).
“When we talk about cancer risk factors, we...sometimes inadvertently put the blame on patients. What I hope [to resolve are] social determinants of health and the ways that stigma and discrimination create the circumstances that drive disease, and thus the ways that we can intervene and decrease cancer risk through trying to affect structural stigma and discrimination. The violence that people experience—the stigma discrimination and violence that people experience—is an issue for oncology,” Alpert concluded
Disease-Specific Barriers in the LGBTQ+ Population
While Alpert’s research focused on how risk factors within the LGBTQ+ community may put them at a higher risk to develop cancer, Gwendolyn P. Quinn, PhD, professor in the Departments of Obstetrics and Gynecology and of Population Health at New York University (NYU) Grossman School of Medicine of NYU Langone Health, noted how increased risk factors could lead to specific diseases within the population.5
She emphasized that although the LGBTQ+ population isn’t at greater risk of developing cancer compared with heterosexual populations, she emphasized that certain cancer risk factors, such as alcohol and tobacco use, are more common. Moreover, evidence has indicated that these individuals may be less likely to seek preventative medical care in a timely manner due, in part, to the risk of discrimination.6
Supporting this theory, findings have indicated that gay and bisexual women may be at a higher risk for developing breast cancer due to their being more likely to be nulliparous and obese. Similarly, gay men could be at higher risk of developing anal cancer due to higher rates of HPV infection, a casual risk factor, in that population.7
HPV also plays an important role in the development of other diseases such as cervical cancer, with research indicating that the disease might be common among lesbians than had been previously understood. In terms of other gynecologic cancers, endometrial cancer is suggested to be more prevalent in lesbians than heterosexual women due to a higher prevalence of nulliparity and a trend towards a higher BMI. Quinn stated that lack of awareness around screening needs is another factor that could lead to a higher prevalence of endometrial cancer in this population.
Although certain cancer risks appear to be elevated within LGBTQ+ populations, a national cancer registry that collects sexual orientation and gender identity data is lacking. In a discussion with CancerNetwork®, Quinn went into detail about the importance of collecting gender identity and sexuality data within the oncology space.
“In a session [at the ASCO Annual Meeting], someone mentioned that they were living in a rural area and that collecting sexual orientation and gender identity data could be off-putting to the majority of their group and very polarizing,” she said. “[We] have to normalize this for everybody, not just [LGBTQ+ people]. Heterosexual people wonder why they’re being asked [these questions, and] queer people [also] wonder why they’re being asked. There’s a lack of knowledge as to why this is important.”
She emphasized that there is a lack of understanding among patients of all sexual orientations and gender identities as to the importance of these questions and that normalizing questions around these factors the same as race/ethnicity data or socioeconomic information is a good place to start. Once that information is disclosed, it is important to give care that takes gender identity and sexual orientation data into consideration to ensure the best quality of care, she stated.
References
- Alpert AB, Sayegh SJ, Strawderman MS, et al. Cancer risk factors and cancer in transgender versus cisgender people: real-world data from a tertiary health care institution. J Clin Oncol. 2022;40(suppl 16):6538. doi:10.1200/JCO.2022.40.16_suppl.6538
- 2022 U.S. Trans Survey. National Center for Transgender Equality. Accessed June 24, 2022. https://bit.ly/3zW825x
- Alpert AB, Sayegh SJ, Strawderman MS, et al. Associations between interpersonal violence and cancer risk factors for transgender and cisgender people. J Clin Oncol. 2022;40(suppl 16):6516. doi:10.1200/JCO.2022.40.16_suppl.6516
- Quinn GP. Gynecologic cancer barriers in the LGBTQ+ community. Presented at: 2022 American Society of Clinical Oncology Annual Meeting; June 3-7; Chicago, IL.
- Kamen CS, Alpert A, Margolies L, et al. "Treat us with dignity": a qualitative study of the experiences and recommendations of lesbian, gay, bisexual, transgender, and queer (LGBTQ) patients with cancer. Support Care Cancer. 2019;27(7):2525-2532. doi:10.1007/s00520-018-4535-0
- Quinn GP, Sanchez JA, Sutton SK, et al. Cancer and lesbian, gay, bisexual, transgender/transsexual, and queer/questioning populations (LGBTQ). CA Cancer J Clin. 2015;65(5):384-400. doi:10.3322/caac.21288