Full-Spectrum Colonoscopy Decreased Adenoma Miss Rate
The use of full-spectrum colonoscopy significantly decreased the number of adenomas missed during an examination compared with the use of forward-viewing colonoscopy, according to the results of an international, multicenter study.
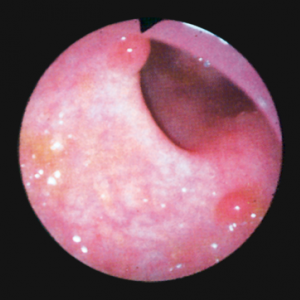
Small adenomas seen with standard colonoscopy
The use of full-spectrum colonoscopy significantly decreased the number of adenomas missed during an examination compared with the use of forward-viewing colonoscopy, according to the results of an international, multicenter study published in the Lancet Oncology.
The trial was conducted by Ian M. Gralnek, MD, of Rambam Health Care Campus, Haifa, Israel, and colleagues to determine if full-spectrum colonoscopy, which images on the forward tip and both side tips of the colonoscope, could reduce the adenoma miss rate of colonoscopy procedures. A reduction in this miss rate could reduce the occurrence of interval colorectal cancers.
The study was conducted in Israel, the Netherlands, and the United States, and included 197 patients aged 18 to 70 years who were referred for colorectal cancer screening, polyp surveillance, or diagnostic assessment; 185 patients were included in the per-protocol analysis. The patients were randomly assigned to receive back-to-back tandem colonoscopy with either forward-viewing colonoscopy (n = 88) first or full-spectrum colonoscopy (n = 97) first.
Overall, the adenoma miss rate was significantly lower in the full-spectrum group compared with the forward-viewing group. Using forward-viewing technology 41% of adenomas were missed compared with 7% using the full-spectrum technology (P < .0001).
Forward-viewing colonoscopy was found to have missed 20 adenomas in 15 patients, 15% of which were advanced stage. Full-spectrum missed five adenomas in five patients, but none were advanced stage.
In an accompanying editorial, David F. Ransohoff, MD, of the divisions of gastroenterology and hepatology at the University of North Carolina at Chapel Hill, wrote that the wider field of view made available through full-spectrum colonoscopy would be appealing to clinicians.
“Outcomes will probably be improved by detection of otherwise missed important lesions that might grow to advanced cancer before a second examination, such as large advanced adenomas and early cancer,” Ransohoff wrote. “Data from Gralnek and colleagues’ study cannot directly address improved detection of those lesions, but this technology could help, particularly for lesions in the right colon that are subtle and flat, and for those behind folds.”
However, Ransohoff also pointed out that this more sensitive technology might have some downsides, specifically when dealing with smaller lesions sized 1 mm to 5 mm.
“With diminutive and small lesions making up most of the identified lesions, some endoscopists report detection of up to 50% or 60% with current technologies,” he wrote. “We need to consider, therefore, how management of small adenomas can affect outcomes, including how an approach can eventually be tailored to small adenomas that maximizes benefit while minimizing effort and possible harm.”