Gemtuzumab-Ozogamicin Improves EFS in Young AML Patients
The addition of gemtuzumab-ozogamicin to standard chemo improved event-free survival in children and young adults with newly diagnosed acute myeloid leukemia.
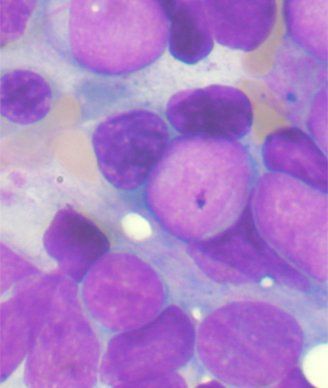
Bone marrow aspirate showing AML; source: Tontoni, Wikimedia Commons
The addition of gemtuzumab-ozogamicin to standard chemotherapy improved event-free survival in children and young adults with newly diagnosed acute myeloid leukemia (AML), according to a new study. Overall survival was not significantly improved, however.
The study was led by Alan S. Gamis, MD, MPH, of Children’s Mercy Hospitals in Kansas City, Missouri, and included 1,022 AML patients ages 0 to 29 years. Patients were randomized to receive either standard chemotherapy (511 patients), or standard chemotherapy plus gemtuzumab-ozogamicin (GO; 511 patients), which targets CD33. Results were published online ahead of print last week in the Journal of Clinical Oncology.
After 3 years, the event-free survival rate was 53.1% for the GO group and 46.9% for the chemotherapy group, for a hazard ratio (HR) of 0.83 (95% CI, 0.70-0.99; P = .04). Overall survival was no different, at 69.4% for GO and 65.4% for chemotherapy alone, an HR of 0.91 (95% CI, 0.74-1.13; P = .39).
“We identified that this benefit was manifested more by a reduction in relapse than in improvement in remission,” Gamis said in an e-mail. Remission rates were 88% and 85% (P = .15), while a post-hoc analysis showed 3-year relapse risk was 32.8% for GO and 41.3% for chemotherapy alone, an HR of 0.73 (95% CI, 0.58-0.91; P = .006).
Gamis said the most surprising findings in the study were that in intermediate risk patients, the benefit seen was restricted to only those who had received a matched stem cell transplant. Also, high-risk patients with a high FLT3-ITD allelic ratio, a mutation associated with high CD33 suppression, saw more benefit than others. He said these two findings are novel and deserve further study.
Importantly, the GO group did have a trend toward increased post-remission toxic mortality, a rate of 6.6% at 3 years compared with 4.1% for an HR of 1.69 (95% CI, 0.93-3.08; P = .09). Gamis said this was primarily in the last two intensification cycles of the treatment, and a new trial eliminating the last cycle hopefully would eliminate the increase in risk.
“This study, in conjunction with several recent adult studies … should reopen the case for bringing this agent back to the patient as an important piece of the overall therapeutic treatment of AML,” Gamis said.
Study Details
The median age at diagnosis was 9.7 years; the biggest group was aged 2 to 10, with 354 patients (34.6% of cohort), and only 13 patients were 21 years or older. Most patients were white (81.3%). More than half of the cohort (607 patients, 59.4%) fell into the intermediate-risk category, followed by low-risk (246 patients, 24.1%) and high-risk (169 patients, 16.5%) groups.