Introduction
Survival of cancer patients has improved dramatically in the past several decades; the 5-year overall survival rate in the United States was 49% in the 1970s but rose to 67% by 2012.[1,2] Advances in cancer survival have exposed risks of death from other causes, such as cardiovascular disease (CVD), the leading cause of death in the United States and the leading cause of death in survivors of early breast cancer.[3-5] Cancer treatments such as systemic therapy (not only with traditional chemotherapy but also with targeted agents and immunotherapy) and radiation therapy induce myriad cardiac toxicities that are frequently underappreciated. Here, we discuss the etiologies, prevention, and management of cardiac toxicities in cancer survivors, considering cancer-related, treatment-related, and patient-related risks and effects. Programs in place to address cardiovascular risk factors in cancer survivors are highlighted.
Cancer as a Cardiotoxic State
Cancer and CVD share common risk factors that induce inflammation and oxidative stress.[6] Inflammation, a hallmark of cancer, not only triggers mutagenesis and contributes to cancer pathophysiology,[7-9] but also is associated with cardiac disease and atherosclerosis.[10] Chronic systemic inflammation can lead to metabolic dysregulation, atherosclerosis,[11] cachexia and muscle wasting, and impaired regeneration of cardiac muscle.[12] These conditions increase the risk of coronary artery vasospasm, coronary artery disease (CAD), cardiomyopathies, and cardiac ischemia and infarction in cancer survivors.[13] Age-related cardiovascular risk is also a contributing factor: 86% of new cancers diagnosed in the United States occur in patients over age 50, a group already at increased risk for CVD in the general population.[1]
Treatment-Related Cardiotoxicity
The cardiotoxicities of chemotherapy and radiation therapy can be broadly classified as acute or late effects. The acute effects of cancer treatment primarily impact the vascular system, specifically leading to hypertension, vasospasm, and thrombosis (including venous thromboembolic disease and rupture of arterial plaques). Late effects are long-term toxicities that generally involve structural cardiovascular changes, including atherosclerosis, valvular heart disease, and conduction system disease. Chemotherapy-induced cardiomyopathy often occurs during active treatment but may have a delayed onset.
Acute effects
Hypertension is a recognized long-term consequence of exposure to several chemotherapeutic agents.[14] It has also been observed acutely in the context of antiangiogenic therapies. Agents that inhibit vascular endothelial growth factor and its receptors-such as bevacizumab, sunitinib, sorafenib, and pazopanib-cause hypertension in up to 80% of patients.[15,16] The primary etiology of this effect is vasoconstriction through nitric oxide blockade and inhibition of other endothelium-derived vasodilatory factors.[17] The key to its management is patient education and on-treatment monitoring. No specific guidelines exist for initiation or selection of antihypertensive therapy in patients and survivors of cancer. However, it is generally appropriate to adhere to guidelines from the Eighth Joint National Committee,[18] which recommend diuretics, dihydropyridine calcium channel blockers, and angiotensin-converting enzyme inhibitors or angiotensin receptor blockers, taking into account individual patient comorbidities (such as diabetes mellitus, kidney disease). Nonselective beta-blockers such as labetalol and carvedilol are also effective antihypertensive agents that may be especially appropriate in patients with known coronary disease, given their proven efficacy in secondary prevention.[19]
Arterial or venous thrombosis can occur at increased frequency throughout chemotherapeutic treatment and beyond. Arterial thrombotic events most often occur as a consequence of plaque rupture at sites of atherosclerosis, which can exist from baseline disease or develop as a result of radiation therapy.[20] Since cancer is associated with hypercoagulability, cancer survivors are at higher risk of venous thromboembolism, which can be caused by the use of central venous catheters during chemotherapy.[14]
While no precise intervention can completely prevent the formation of blood clots, precautionary measures should be taken to reduce the risk. Cancer patients and survivors should avoid prolonged immobile states without ambulation, and indwelling venous access lines should be regularly maintained and replaced. Additionally, as in patients without cancer, regular exercise, proper nutrition, and avoidance of tobacco are critical lifestyle modifications to reduce the risk and progression of atherosclerosis. Patients with known coronary atherosclerosis should be maintained on low-dose aspirin for primary prevention in the absence of contraindications such as thrombocytopenia. Once a thrombotic event has occurred and been treated appropriately, long-term antithrombotic therapy with aspirin, warfarin, or direct oral anticoagulants should be considered for secondary prevention.[14]
Late effects
Key Points
- The treatment of cancer carries a significant risk for acute and late cardiovascular toxicities.
- Acute toxicities include hypertension, vascular
thrombosis, vasospasm, and myocarditis. - Late toxicities include atherosclerosis, valvular
heart disease, and conduction system disease. - Following a plant-based diet, engaging in regular
aerobic exercise, smoking cessation, and other lifestyle modifications in cancer survivors can mitigate the cardiovascular toxicities.
Accelerated atherosclerosis is frequently seen in cancer survivors, particularly as a late effect of localized radiation therapy. The risk is dependent on the affected vasculature within the radiation field; mediastinal irradiation is associated with CAD,[21] neck irradiation with carotid disease,[22] abdominal irradiation with mesenteric ischemia, and limb irradiation with peripheral vascular disease.[23,24] In patients with concomitant cardiovascular risk factors in addition to a history of radiation therapy, targeted screening tests such as electrocardiograms (ECGs) and echocardiograms, stress testing for CAD, Doppler ultrasound for carotid and peripheral vascular disease, and annual evaluation of lipid profiles and thyroid-stimulating hormone levels may be indicated to provide further risk stratification.[14] If evidence of disease is found, the most effective intervention entails aggressive risk factor management. Pharmacologic therapies include antiplatelet therapy (including aspirin and P2Y12 receptor antagonists when appropriate), statin-based lipid-lowering agents, and antihypertensive therapy. Nonpharmacologic measures include regular aerobic exercise, improved nutrition, and cessation of tobacco and alcohol abuse.[25,26] Cardiovascular mortality is greater in patients whose CAD is associated with radiation therapy rather than CAD associated with atherosclerosis occurring after percutaneous interventions.[27] Accordingly, early detection and initiation of treatment are paramount.
Valvular disease, including both stenosis and regurgitation, occurs most notably after mediastinal radiation.[20] Radiation-induced inflammation leads to fibrotic thickening, valvular retraction, and accelerated calcification.[28] Mild to moderate valvular disease is usually clinically silent unless a patient has limited cardiopulmonary reserve. Therefore, patients should undergo serial assessments with clinical evaluation, ECG, and echocardiography, often in consultation with the cardiology team in order to optimize assessment intervals. If necessary, cardiothoracic surgery team input should be sought for consideration of valve repair or replacement.
Cardiac conduction system disease has also been observed after radiation therapy and chemotherapy. The involved fields in chest and mantle field irradiation invariably envelop some portion of the heart. Progressive radiation-induced cardiac injury may lead to bradyarrhythmias (sick sinus syndrome, atrioventricular block, QT prolongation) and tachyarrhythmias (atrial fibrillation, supraventricular tachycardia).[29,30] Atrial fibrillation can also be provoked by various chemotherapeutic agents, including ibrutinib, cisplatin, docetaxel, fluorouracil, gemcitabine, ifosfamide, and etoposide.[31,32] Symptoms suggestive of a conduction system abnormality, such as palpitations or syncope, should prompt monitoring using an ECG and a Holter monitor or event monitor, as well as a cardiology referral, if appropriate, for further patient evaluation and management. An echocardiogram should be performed for most patients with arrhythmias, and some patients may warrant coronary assessment for ischemia. Electrophysiology referral may be necessary for symptomatic bradyarrhythmias requiring a permanent pacemaker, refractory supraventricular arrhythmias requiring antiarrhythmic agents or ablation, or ventricular arrhythmias requiring an implantable cardioverter-defibrillator.[20]
A well-known long-term complication of anthracyclines and trastuzumab is cardiomyopathy leading to congestive heart failure. The pathophysiology and management of this complication have been discussed extensively throughout the literature.[33-36] Given the increased awareness about the acute and late cardiotoxic effects of cancer treatment modalities, it should be noted that significant changes in practice patterns are likely to shift the spectrum of cardiotoxicity in cancer survivors. The administration of anthracyclines is restricted to lifetime dose limits, and in combined regimens these agents are often replaced by alternatives.[37] In recent years, the use of advanced technologies (intensity-modulated radiation therapy, stereotactic body radiation therapy) has decreased the incidence of unintentional cardiac dosing. These changes are likely to lead to a decreased prevalence of cardiotoxicity among long-term cancer survivors in the coming decades.
Finally, newer treatment modalities such as immune checkpoint inhibition (against cytotoxic T-lymphocyte–associated antigen 4, programmed death 1, and programmed death ligand 1) can cause systemic inflammation and cardiac toxicity, including end-organ myofibrosis, autoimmune myocarditis, and acute heart failure.[38-40] However, in light of the relatively recent advances in development of various immunotherapies, their associated mechanisms of cardiotoxicity need to be explored further.
Cancer Survivorship
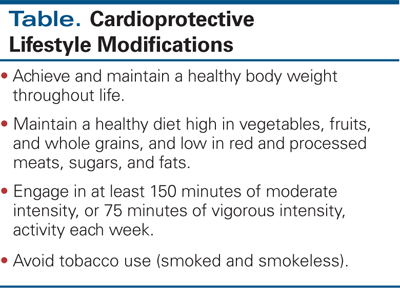
The most broadly effective intervention to address cardiovascular risk factors in cancer survivors is the adoption of healthy lifestyle behaviors as recommended by the American Cancer Society,[41,42] American Society of Clinical Oncology,[43] the National Comprehensive Cancer Network,[44] and the World Health Organization.[45] Each of these organizations recognizes the importance of a plant-based diet and regular physical activity in order to combat treatment-associated metabolic changes and reduce the risk of CAD. Physical activity has been shown to improve cardiovascular fitness in early breast cancer survivors, which results in enhanced daily function and quality of life,[46] and to reduce cardiovascular events among survivors of Hodgkin lymphoma.[47] Although the benefits of lifestyle modifications are intuitive, research is underway to investigate the effects of diet and exercise on cancer recurrence (ClinicalTrials.gov identifier: NCT02750826) and metabolic syndrome.[48] Currently, the National Institutes of Health has a program announcement to further study outcomes in cancer treatment–related cardiotoxicity,[49] including a research focus on behavioral interventions to mitigate or reverse cardiovascular damage.
Conclusion
As the overall survival of patients with cancer continues to rise, more cancer survivors are faced with the risk of developing treatment-related cardiovascular toxicities. Focused early patient evaluation and disease detection can stem the overall progression of cardiovascular-related debilitation, but prior cancer treatments are certainly not the sole culprits. Both cancer and CVD are characterized by a pro-inflammatory, mutagenic state, which can persist into the post-treatment period of survivorship and compound the risks of further cardiovascular decline. An effective approach to addressing cardiovascular toxicity in cancer survivors entails efforts to reduce risk factors through patient education and health promotion; diligent monitoring for early signs of toxicity; and coordinating patient management among the disciplines of oncology, cardiology, and primary care.
Financial Disclosure:The authors have no significant interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. Wolmark N, Wang J, Mamounas E, et al. Preoperative chemotherapy in patients with operable breast cancer: nine-year results from National Surgical Adjuvant Breast and Bowel Project B-18. J Natl Cancer Inst Monogr. 2001;(30):96-102.
2. Howlader N, Noone A, Krapcho M, et al. SEER cancer statistics review, 1975–2013. National Cancer Institute. Bethesda, MD. http://seer.cancer.gov/csr/1975_2013/. Based on November 2015 SEER data submission, posted to the SEER website, April 2016. Accessed November 1, 2016.
3. Patnaik JL, Byers T, DiGuiseppi C, et al. Cardiovascular disease competes with breast cancer as the leading cause of death for older females diagnosed with breast cancer: a retrospective cohort study. Breast Cancer Res. 2011;13:R64.
4. Colzani E, Liljegren A, Johansson AL, et al. Prognosis of patients with breast cancer: causes of death and effects of time since diagnosis, age, and tumor characteristics. J Clin Oncol. 2011;29:4014-21.
5. Writing Group members, Mozaffarian D, Benjamin EJ, Go AS, et al; American Heart Association Statistics Committee; Stroke Statistics Subcommittee. Heart disease and stroke statistics-2016 update: a report from the American Heart Association. Circulation. 2016;133:e38-e360.
6. Koene RJ, Prizment AE, Blaes A, Konety SH. Shared risk factors in cardiovascular disease and cancer. Circulation. 2016;133:1104-14.
7. Diakos CI, Charles KA, McMillan DC, Clarke SJ. Cancer-related inflammation and treatment effectiveness. Lancet Oncol. 2014;15:e493-e503.
8. Colotta F, Allavena P, Sica A, et al. Cancer-related inflammation, the seventh hallmark of cancer: links to genetic instability. Carcinogenesis. 2009;30:1073-81.
9. Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144:646-74.
10. Libby P. Inflammation in atherosclerosis. Nature. 2002;420:868-74.
11. Whitlock MC, Yeboah J, Burke GL, et al. Cancer and its association with the development of coronary artery calcification: an assessment from the multi-ethnic study of atherosclerosis. J Am Heart Assoc. 2015;4.
12. Talbert EE, Guttridge DC. Impaired regeneration: a role for the muscle microenvironment in cancer cachexia. Semin Cell Dev Biol. 2016;54:82-91.
13. Khakoo AY, Yeh ET. Therapy insight: Management of cardiovascular disease in patients with cancer and cardiac complications of cancer therapy. Nat Clin Pract Oncol. 2008;5:655-67.
14. Lenihan DJ, Cardinale DM. Late cardiac effects of cancer treatment. J Clin Oncol. 2012;30:3657-64.
15. Yang JC, Haworth L, Sherry RM, et al. A randomized trial of bevacizumab, an anti-vascular endothelial growth factor antibody, for metastatic renal cancer. N Engl J Med. 2003;349:427-34.
16. Patel TV, Morgan JA, Demetri GD, et al. A preeclampsia-like syndrome characterized by reversible hypertension and proteinuria induced by the multitargeted kinase inhibitors sunitinib and sorafenib. J Natl Cancer Inst. 2008;100:282-4.
17. Robinson ES, Khankin EV, Karumanchi SA, Humphreys BD. Hypertension induced by vascular endothelial growth factor signaling pathway inhibition: mechanisms and potential use as a biomarker. Semin Nephrol. 2010;30:591-601.
18. James PA, Oparil S, Carter BL, et al. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA. 2014;311:507-20.
19. Bangalore S, Steg G, Deedwania P, et al. Beta-blocker use and clinical outcomes in stable outpatients with and without coronary artery disease. JAMA. 2012;308:1340-9.
20. Jaworski C, Mariani JA, Wheeler G, Kaye DM. Cardiac complications of thoracic irradiation. J Am Coll Cardiol. 2013;61:2319-28.
21. Heidenreich PA, Schnittger I, Strauss HW, et al. Screening for coronary artery disease after mediastinal irradiation for Hodgkin’s disease. J Clin Oncol. 2007;25:43-9.
22. Moritz MW, Higgins RF, Jacobs JR. Duplex imaging and incidence of carotid radiation injury after high-dose radiotherapy for tumors of the head and neck. Arch Surg. 1990;125:1181-3.
23. Sanon S, Lenihan DJ, Mouhayar E. Peripheral arterial ischemic events in cancer patients. Vasc Med. 2011;16:119-30.
24. Javid M, Magee TR, Galland RB. Arterial thrombosis associated with malignant disease. Eur J Vasc Endovasc Surg. 2008;35:84-7.
25. Alfano CM, Ganz PA, Rowland JH, Hahn EE. Cancer survivorship and cancer rehabilitation: revitalizing the link. J Clin Oncol. 2012;30:904-6.
26. McCullough LE, Eng SM, Bradshaw PT, et al. Fat or fit: the joint effects of physical activity, weight gain, and body size on breast cancer risk. Cancer. 2012;118:4860-8.
27. Reed GW, Masri A, Griffin BP, et al. Long-term mortality in patients with radiation-associated coronary artery disease treated with percutaneous coronary intervention. Circ Cardiovasc Interv. 2016;9:e003483.
28. Wethal T, Lund MB, Edvardsen T, et al. Valvular dysfunction and left ventricular changes in Hodgkin’s lymphoma survivors. A longitudinal study. Br J Cancer. 2009;101:575-81.
29. Galper SL, Yu JB, Mauch PM, et al. Clinically significant cardiac disease in patients with Hodgkin lymphoma treated with mediastinal irradiation. Blood. 2011;117:412-8.
30. Larsen RL, Jakacki RI, Vetter VL, et al. Electrocardiographic changes and arrhythmias after cancer therapy in children and young adults. Am J Cardiol. 1992;70:73-7.
31. van der Hooft CS, Heeringa J, van Herpen G, et al. Drug-induced atrial fibrillation. J Am Coll Cardiol. 2004;44:2117-24.
32. McMullen JR, Boey EJ, Ooi JY, et al. Ibrutinib increases the risk of atrial fibrillation, potentially through inhibition of cardiac PI3K-Akt signaling. Blood. 2014;124:3829-30.
33. Ewer MS, Ewer SM. Cardiotoxicity of anticancer treatments. Nat Rev Cardiol. 2015;12:547-58.
34. Fanous I, Dillon P. Cancer treatment-related cardiac toxicity: prevention, assessment and management. Med Oncol. 2016;33:1-11.
35. Zagar TM, Cardinale DM, Marks LB. Breast cancer therapy-associated cardiovascular disease. Nat Rev Clin Oncol. 2016;13:172-84.
36. Gupta D, Chan A, Jordan J, Steingart RM. Chemotherapy-induced cardiomyopathy: clinical scenarios and challenges. Oncology (Williston Park). 2015;29:730-2,86.
37. Giordano SH, Lin YL, Kuo YF, et al. Decline in the use of anthracyclines for breast cancer. J Clin Oncol. 2012;30:2232-9.
38. Läubli H, Balmelli C, Bossard M, et al. Acute heart failure due to autoimmune myocarditis under pembrolizumab treatment for metastatic melanoma. J Immunother Cancer. 2015;3:11.
39. Koelzer VH, Rothschild SI, Zihler D, et al. Systemic inflammation in a melanoma patient treated with immune checkpoint inhibitors-an autopsy study. J Immunother Cancer. 2016;4:13.
40. Johnson DB, Balko JM, Compton ML, et al. Fulminant myocarditis with combination immune checkpoint blockade. N Engl J Med. 2016;375:1749-55.
41. Kushi LH, Doyle C, McCullough M, et al. American Cancer Society Guidelines on nutrition and physical activity for cancer prevention: reducing the risk of cancer with healthy food choices and physical activity. CA Cancer J Clin. 2012;62:30-67.
42. Rock CL, Doyle C, Demark-Wahnefried W, et al. Nutrition and physical activity guidelines for cancer survivors. CA Cancer J Clin. 2012;62:243-74.
43. Runowicz CD, Leach CR, Henry NL, et al. American Cancer Society/American Society of Clinical Oncology Breast Cancer Survivorship Care Guideline. J Clin Oncol. 2016;34:611-35.
44. National Comprehensive Cancer Network. NCCN Guidelines: Survivorship. Version 1.2016. https://www.nccn.org/professionals/physician_gls/pdf/survivorship.pdf. Accessed November 1, 2016.
45. World Health Organization. The World Health Organization’s fight against cancer: strategies that prevent, cure and care. Geneva, Switzerland. 2007. http://www.who.int/cancer/publicat/WHOCancerBrochure2007.FINALweb.pdf. Accessed October 28, 2016.
46. Casla S, Lopez-Tarruella S, Jerez Y, et al. Supervised physical exercise improves VO2max, quality of life, and health in early stage breast cancer patients: a randomized controlled trial. Breast Cancer Res Treat. 2015;153:371-82.
47. Jones LW, Liu Q, Armstrong GT, et al. Exercise and risk of major cardiovascular events in adult survivors of childhood Hodgkin lymphoma: a report from the childhood cancer survivor study. J Clin Oncol. 2014;32:3643-50.
48. Dieli-Conwright CM, Mortimer JE, Schroeder ET, et al. Randomized controlled trial to evaluate the effects of combined progressive exercise on metabolic syndrome in breast cancer survivors: rationale, design, and methods. BMC Cancer. 2014;14:238.
49. Department of Health and Human Services. National Institutes of Health. Improving outcomes in cancer treatment-related cardiotoxicity (R01). http://grants.nih.gov/grants/guide/pa-files/PA-16-035.html. Accessed October 31, 2016.