HPV, p16 Associated With Outcomes in Anal Canal Carcinoma
Expression of the p16 tumor suppressor was found to be a prognostic factor for survival in patients with carcinoma of the anal canal.
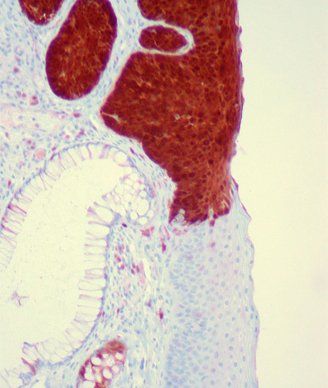
Anal squamous carcinoma in situ, p16 immunostain; source; Ed Uthman, Wikimedia Commons
Expression of the tumor suppressor p16 was found to be a significant, independent prognostic factor for both overall and disease-specific survival in patients with stages I–III carcinoma of the anal canal. The new retrospective study also found some correlation with outcome and positivity of a high-risk subtype of human papillomavirus (HPV).
Anal carcinomas are rare, with, an incidence of only 1 to 2.5 cases per 100,000 people per year in many countries, and HPV is among the primary risk factors for the disease. “Among more than 130 different HPV subtypes, HPV16 is the most prevalent in anal carcinoma and is present in up to 89% of all patients with anal carcinoma,” wrote study authors led by Eva Serup-Hansen, MD, PhD, of Copenhagen University Hospital Herlev in Denmark. There is also a high correlation between HPV16 and p16 positivity (which is used as a marker for HPV status), though few studies have looked at these as prognostic factors for outcome in anal carcinoma.
The new study included retrospective analyses of 143 patients with anal carcinoma, and involved genotyping of HPV high-risk subtypes and immunohistochemical analysis of p16 expression; all patients were treated with either combined chemoradiotherapy or radiotherapy alone. The results were published online ahead of print on May 12 in the Journal of Clinical Oncology.
HPV16 was found in 81% of tumors, far and away the most common of the HPV subtypes; it was followed by HPV33, present in only 5.1% of tumors, and HPV18 and HPV58 in even fewer patients. Also, p16 positivity was seen in 92.9% of tumors.
Both HPV positivity and p16 positivity were correlated with significantly improved overall survival (OS) and disease-specific survival (DSS). After a median follow-up of 51.2 months, HPV-positive patients had an OS of 74% compared with 52% for HPV-negative patients (P = .036), and a DSS of 84% vs 52% (P = .002); p16-positive patients also had better OS (76% vs 30%; P < .001) and DSS (85% vs 30%; P < .001) than p16-negative patients.
On a multivariable analysis that accounted for HPV status, p16 status, sex, T stage, N stage, and treatment, only p16 positivity remained an independent prognostic factor for OS and DSS. The hazard ratio for p16-positive patients for OS was 0.07 (95% CI, 0.01-0.61; P = .016); for DSS it was also 0.07 (95% CI, 0.01-0.53; P = .011).
“We found that p16 positivity was a strong independent prognostic factor for improved OS and DSS in patients with anal carcinoma,” the authors concluded. Because the p16-negative tumors likely have different tumor biology, they wrote that future studies should consider stratifying patients according to p16 status. “This might select candidates for a more rigorous follow-up and facilitate initiation of studies with alternative treatment regimens for this prognostically unfavorable group.”