Idelalisib Improves Outcomes in Leukemia and Lymphoma
The combination of idelalisib with rituximab improved survival in relapsed CLL, and idelalisib also showed antitumor activity as a single agent in patients with indolent non-Hodgkin lymphoma.
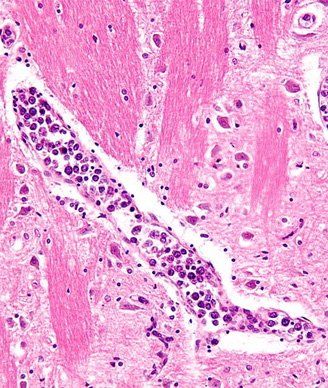
High magnification micrograph of an intravascular lymphoma in blood vessels of the pons. Copyright 2010 Nephron.
The combination of idelalisib and the anti-CD20 antibody rituximab improved response rates, progression-free survival, and overall survival in patients with relapsed chronic lymphocytic leukemia (CLL) over rituximab alone. Idelalisib also showed antitumor activity as a single agent in patients with indolent non-Hodgkin lymphoma (NHL) who had received extensive prior therapies. Both of these studies are published in the New England Journal of Medicine.
“The addition of idelalisib to rituximab in a population of frail, difficult-to-treat patients, including those with adverse genetic features, such as 17p deletion, TP53 mutations, or unmutated IGHV, was superior to rituximab monotherapy, which is commonly used in such patients,” concluded the study authors.
Idelalisib is a first-in-class oral kinase inhibitor of phosphoinositide 3-kinase (PI3K) delta, in development by California-based Gilead Sciences. The delta isoform of the PI3K is found predominantly in leukocytes but not other cell types. Gilead submitted a New Drug Application (NDA) to the US Food and Drug Administration (FDA) for approval of idelalisib based on both the CLL and NHL studies. The FDA accepted the NHL filing on January 13, and a decision is expected in September. Idelalisib was granted a breakthrough therapy designation for CLL following the NDA submission for NHL.
Initial results from these two studies were first presented at last year’s American Society of Hematology (ASH) Annual Meeting and Exposition.
The newly published results of the phase III randomized Study 116 show that the median progression-free survival is 5.5 months in the rituximab plus placebo control arm and has not yet been reached in the experimental idelalisib arm (hazard ratio [HR] for progression or death in the idelalisib group was 0.15; P < .001). At 24 weeks, the progression-free survival rate was 93% and 46% in the idelalisib and control groups, respectively.
Patients treated with idelalisib had an overall response rate of 81% compared with 13% in the control arm (P < .001). The 12-month overall survival rate was 92% in the experimental arm compared with 80% in the control arm (HR for death was 0.28; P = .02).
The trial included 220 CLL patients with decreased renal function and previous therapy–induced myelosuppression or major coexisting illnesses who were not eligible for chemotherapy following progression. Patients were randomized 1:1 to receive either eight infusions of rituximab and either placebo or a 150-mg dose of idelalisib twice daily. Seventy-eight percent of patients were older than 65, and 40% had at least moderate renal insufficiency.
Serious adverse events occurred in 40% of the patients in the experimental treatment arm and in 35% of those in the control arm.
Based on a recommendation of the Data and Safety Monitoring Board, the study was stopped early at the first prespecified interim analysis due to efficacy.
“Patients with relapsed CLL have limited treatment options and are often not able to tolerate chemotherapy,” said Richard R. Furman, MD, of the division of hematology/oncology at the Weill Cornell Medical Center and New York-Presbyterian Hospital, in a previous statement. “Based upon the results of this study demonstrating significant improvements in progression-free and overall survival, idelalisib represents an important addition to the armamentarium for patients living with this life-threatening disease.”
In the second single-arm indolent NHL clinical trial, idelalisib demonstrated activity in a patient population that was refractory to rituximab therapy and to alkylating chemotherapy agents, said the study authors. A total of 125 patients who had relapsed on either chemotherapy or rituximab were enrolled to receive 150-mg idelalisib twice a day.
The response rate was 57% (71 of 125 patients). Six percent of the patients met the criteria for a complete response. The median duration of response was 12.5 months, with a median time to response of 1.9 months. The median progression-free survival was 11 months. The responses were similar for all subtypes of indolent NHL.
Common high-grade adverse events included neutropenia (27% of patients), elevations in aminotransferase levels (13%), diarrhea (13%), and pneumonia (7%).
“In this uncontrolled trial, idelalisib targets the PI3K delta pathway and appears to provide effective oral monotherapy in patients with previously treated indolent non-Hodgkin lymphoma. The toxicity profile does not generally overlap with that of most other active agents and may allow the development of more highly active combination regimens,” concluded study coauthor Ajay Gopal, MD, of the University of Washington School of Medicine and Seattle Cancer Care Alliance.
Targeted Therapy First Strategy Reduces Need for Chemotherapy in Newly Diagnosed LBCL
December 7th 2025Lenalidomide, tafasitamab, rituximab, and acalabrutinib alone may allow 57% of patients with newly diagnosed LBCL to receive less than the standard number of chemotherapy cycles without compromising curative potential.