Immune Cells, Cytokines Predict Recurrence in Stage I Lung Adenocarcinoma
Expression of certain immune markers in tumor and surrounding cells can help predict probabilities of recurrence in patients with stage I lung adenocarcinoma, according to new researcher.
Expression of certain immune markers in tumor and surrounding cells can help predict probabilities of recurrence in patients with stage I lung adenocarcinoma, according to new work by researchers at Memorial Sloan-Kettering Cancer Center in New York.
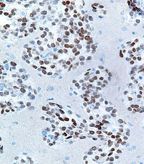
High magnification micrograph of a primary lung adenocarcinoma showing nuclear staining with a TTF-1 immunostain; source: Nephron, Wikimedia Commons
According to senior author Prasad S. Adusumilli, MD, the presence of a “good” immune response can apparently help prevent the cancer’s recurrence. In the new study, Adusumilli and colleagues looked for eight tumor-infiltrating immune cells as well as five cytokines in 956 patients with stage I lung adenocarcinoma; the first 478 patients were considered a training cohort, and the second group of 478 was a validation cohort. The results were published online ahead of print on December 26 in the Journal of Clinical Oncology.
Among the immune cells, a high density of FoxP3-positive cells in the tumor-associated stroma was significantly associated with recurrence (P = 0.43 vs low density). The ratio of FoxP3 to CD3 cells was an even stronger predictor, however; the 5-year recurrence-free probability was 85% for those with a high ratio and 77% for those with a low ratio (P = 0.004). This result was replicated from the training cohort to the validation cohort.
Of the cytokines tested, several were found to have prognostic value. Higher expression levels of interleukin-12 receptor beta-2 (IL-12RB2) was associated with better recurrence rates than lower expression, with a 5-year recurrence-free probability of 90% for the former and 80% for the latter (P = 0.026). In contrast, high expression of tumor IL-7R yielded a poorer 5-year recurrence-free probability of 76% vs 86% for those with lower expression of the cytokine (P = 0.001). These results were also replicated in the validation cohort after first appearing in the training cohort. The other three cytokines tested-CCR7, CXCL12, and CXCR4-showed no significant associations with recurrence.
Multivariate analysis showed that these three immune markers-stromal FoxP3-CD3 ratio, IL-12RB2, and IL-7R-are independently associated with recurrence. The FoxP3-CD3 ratio had a hazard ratio (HR) for recurrence of 2.00 (95% CI, 1.22–3.27; P = 0.006). The two cytokines had HRs of 2.24 (95% CI, 1.02–4.95; P = 0.045) and 1.65 (95% CI, 1.02–2.68; P = 0.45), respectively.
The authors wrote that the current system for evaluating of stage I disease relies only on anatomic factors. “In fact, for stage I lung adenocarcinoma, tumor size is the only standard prognosticator available,” they wrote. “In our study, we have demonstrated the prognostic power of immunologic parameters for stage I lung adenocarcinoma.”
Notably, when overall survival was used as an endpoint rather than recurrence, only IL-7R remained a significant prognosticator (P = 0.007). “The ability of IL-7R to prognosticate both recurrence-free and overall survival merits further investigation of its biologic role,” the authors wrote.