Immune checkpoint inhibitors have demonstrated efficacy across many cancer types in numerous clinical trials. However, because patients with preexisting autoimmune disease were excluded from these seminal trials, there are serious gaps in knowledge regarding the efficacy-and in particular the safety-of these transformative agents in patients with autoimmune disease. The safety of immune checkpoint inhibitors in this population has been an important concern, since these agents unleash immune activation, a potentially dangerous situation for patients with already heightened and aberrant immune function. Several retrospective studies have begun to address this question, finding that autoimmunity is often exacerbated by immune checkpoint inhibitor therapy, but is generally manageable with standard treatment algorithms and close multidisciplinary monitoring. Further, the activity of these agents appears to be comparable to that seen in unselected patients. Here we detail the experience with immune checkpoint inhibitors in patients with autoimmune disease.
Introduction
The advent of effective immunotherapy using immune checkpoint inhibitors has transformed the therapeutic landscape for many cancers. Agents targeting cytotoxic T-lymphocyte–associated antigen 4 (CTLA-4), programmed death 1 (PD-1), and its ligand (PD-L1) unleash key negative regulators of immune activation, thus “removing the brakes” on an effective antitumor immune response. They offer the possibility of previously unheard-of long-term therapeutic benefit for patients with metastatic solid tumors.
Because of the mechanism of action of these therapies, their toxicities are related to aberrant activation of immune cells against self-antigens. These side effects, termed “immune-related adverse events” (irAEs), may affect and inflame essentially any organ. Anti–CTLA-4 antibodies most frequently induce colitis, hepatitis, hypophysitis, thyroiditis, and dermatitis, with severe effects occurring in approximately one-third of patients.[1] Anti–PD-1 agents have similar, albeit less frequent toxicities, and may also cause pneumonitis, inflammatory arthritis, and other adverse effects.[2] Recent studies have also shown that these agents may occasionally cause systemic syndromes that are seemingly identical to known rheumatologic disorders (eg, Sjögren syndrome, sarcoidosis).[3,4] Although these side effects can typically be managed with corticosteroids and other immunosuppressants, highly morbid and even fatal events can occur in a small proportion of patients.[5] Predicting which patients will experiences irAEs and mitigating the risk of severe organ injury remain critical and unmet needs (Figure).
While the molecular characteristics of irAEs are still being unraveled, it is evident that the clinical and histopathologic presentation of these events has a strong resemblance to autoimmune disease. Early insights into their pathogenesis have demonstrated T-cell and macrophage infiltration into the inflamed tissue, as well as autoantibody and antibody-complement deposition in some cases.[5-7] For this reason, it has been of concern that patients with preexisting autoimmune disease would experience flares in their underlying condition when treated with immune checkpoint inhibitors. Further, one could hypothesize that patients prone to autoimmunity might have additional organ inflammation triggered when exposed to this therapy.
An additional source of concern is the fact that there is a wealth of literature documenting the critical role of both CTLA-4 and PD-1 in autoimmunity and in maintaining immune tolerance to self-antigens.[8] Knockout mice designed to genetically lack these molecules develop fulminant and fatal multiorgan autoimmunity (CTLA-4 knockout)[9]; or either myocarditis, cardiomyopathy, or a lupus-like syndrome (PD-1 knockout).[10,11] Moreover, CTLA-4 agonists (abatacept, belatacept) are approved for the treatment of various autoimmune diseases. These concerns have led to the exclusion of patients with autoimmune disease from seminal immune checkpoint inhibitor studies. Thus, when facing a patient with active autoimmune disease and metastatic cancer, a clinician is confronted with a significant dilemma, and a lack of prospective data to inform the safety of treatment.
However, subsequent experience has suggested that the relationship between autoimmunity and immunotherapy is not straightforward. The current data regarding this relationship are not derived from large prospective studies, but rather from retrospective series and case reports. Still, they do provide insights for clinicians and can help them with treatment decision making, and with balancing the competing risks of metastatic cancer and autoimmune disorders.
Ipilimumab and Autoimmune Disease
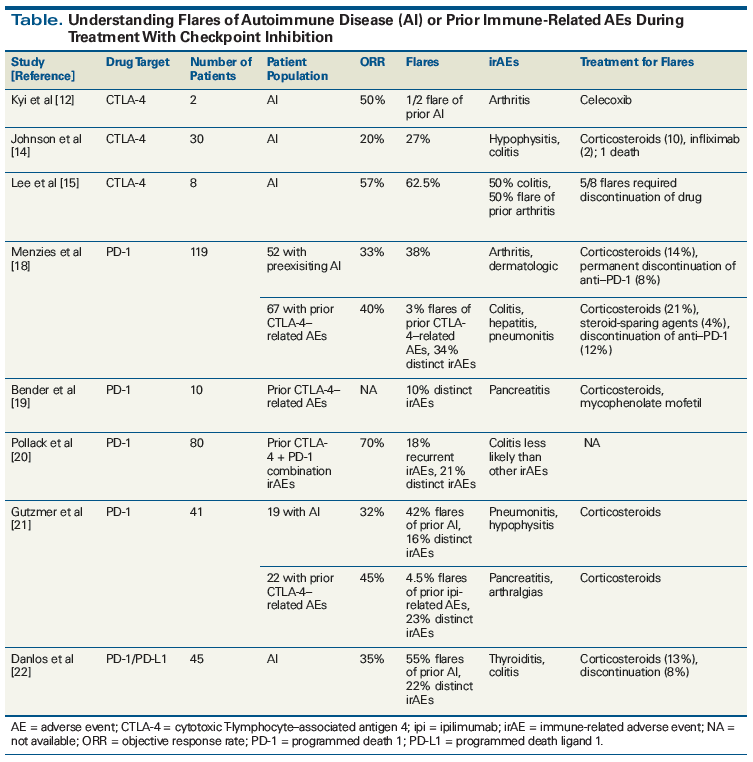
Ipilimumab is approved for use in advanced melanoma at a lower dose (3 mg/kg) and as adjuvant therapy for patients at high risk for recurrence at a high dose (10 mg/kg). Several case reports have suggested that patients with autoimmune disease might tolerate ipilimumab safely and could potentially benefit from therapy.[12,13] To provide additional insights, our group performed a retrospective study of 30 patients with autoimmune disease from 9 centers. These patients had a wide range of diseases, most commonly inflammatory bowel disease (n = 6), rheumatoid arthritis (n = 6), and psoriasis (n = 5). Of these patients, 27% experienced autoimmune exacerbations and 33% had standard irAEs (Table).[14] All of these events were manageable with corticosteroid treatment, infliximab, and/or discontinuation of ipilimumab, except for one patient with pre-existing psoriasis in whom colitis developed and became fatal after a long delay in seeking care. Several patients with inflammatory bowel disease had flares. Half of patients experienced no toxicities and 20% responded to treatment. An additional series of 8 patients with rheumatoid arthritis demonstrated frequent but manageable arthritis flares (25% with grade 3), frequent colitis (50%; all resolved with treatment), and high response rates (50%).[15] From these studies, we conclude that autoimmune disease is not an absolute contraindication to ipilimumab therapy, as long as close clinical monitoring is provided. We would be hesitant, however, to offer high-dose therapy (10 mg/kg), a more toxic regimen, in the adjuvant setting (particularly with the availability of adjuvant nivolumab currently). For patients with more severe autoimmune disease (eg, Guillain Barré syndrome), we would also have an extended discussion of potential life-threatening consequences.
Anti–PD-1/PD-L1 Therapy in Autoimmune Disease
The need to use anti–PD-1/PD-L1 agents in patients with metastatic cancer and autoimmune disease is a much more common scenario. These therapies are approved in numerous solid and hematologic cancers and are rapidly becoming a pillar of cancer therapy. One study that used the Surveillance, Epidemiology, and End Results database estimated that up to 14% of lung cancer patients had some type of autoimmune disorder, demonstrating the frequency of this clinical scenario.[16] Thus, it is essentially inevitable that practicing oncologists will encounter patients with autoimmune disease who might benefit from anti–PD-1/PD-L1 therapy.
The first hints that this might be a tolerable strategy came from patients with melanoma who had previously experienced irAEs with ipilimumab. A phase III study of nivolumab in patients whose disease had previously progressed on ipilimumab demonstrated that reactivation of ipilimumab toxicities did not occur in the vast majority of cases.[17] Retrospective series, which focused only on patients with more severe ipilimumab toxicities, echoed these findings.[18,19] Moreover, our group observed that most cases of toxicities that occurred with combined ipilimumab and nivolumab did not recur with anti–PD-1 rechallenge; this was particularly true of colitis.[20] The data from these studies also support the premise that autoimmune toxicities from these therapies are complex, and are not automatically triggered by anti–PD-1/PD-L1 therapy.
Several subsequent studies have specifically evaluated patients with autoimmune disease treated with anti–PD-1/PD-L1 agents. In one group of 52 melanoma patients with various autoimmune diseases, 38% had autoimmune flares (only 2 discontinued treatment) and 29% had other irAEs.[18] Interestingly, “rheumatoid”-type diseases (rheumatoid arthritis, psoriasis, polymyalgia rheumatica) demonstrated a high likelihood of flares, whereas no patients with gastrointestinal or neurologic autoimmune disorders experienced exacerbations. No patients died from toxicities and 40% of patients responded to treatment. Notably, patients who remained on immunosuppressive treatment when starting anti–PD-1 therapy had lower response rates than untreated patients (15% vs 44%). Other studies have demonstrated similar findings, including a series of 19 patients with melanoma, and a series of 45 patients with various advanced cancers.[21,22] The latter study suggested that survival was similar in patients with and without irAEs/autoimmune flares. However, another study suggested that toxicities appeared less severe in patients who maintained their immunosuppressive treatment.[23] In our experience and in published literature, the autoimmune flares tend to be a worsening of existing disease manifestations rather than a totally new clinical presentation. Despite the largely positive outcomes of these studies, it is not clear that the rate of life-threatening and fatal complications is negligible; one meta-analysis showed that 3 of 123 patients had lethal toxicities.[23,24]
In light of the available evidence, we regard autoimmune disease as an important consideration, but not a contraindication to anti–PD-1/PD-L1 therapy. A thorough discussion with patients is needed prior to initiation of treatment, in which the point must be made that the risk of autoimmune flares is very real, but that these tend to be manageable with vigilant clinical monitoring and standard immunosuppressive treatment regimens. We also attempt to wean patients off of immunosuppressive therapies prior to the start of anti–PD-1/PD-L1 therapy when possible, given the inferior outcomes in patients still receiving immunosuppressants in our retrospective study (although this approach could potentially exacerbate toxicities).[18,23] We consider physiologic doses of corticosteroids, as well as other agents with minimal T-cell effects (hydroxychloroquine, rituximab), as potentially preferable to biologics such as infliximab. While the “optimal” immunosuppressive regimen in this setting is unknown, the published literature seems to suggest both decreased efficacy and decreased toxicity for patients receiving immunosuppression. Co-managing these patients with a rheumatologist may be helpful. Indeed, multidisciplinary, collaborative, and communicative care is absolutely essential in these complicated cases.
KEY POINTS
- Immune checkpoint inhibitors unleash quiescent and exhausted immune responses, presenting a challenge for patients with dysregulated immunity, particularly those with autoimmune disease.
- Retrospective studies suggest that many patients do have flares in their underlying autoimmune disease when treated with immune checkpoint inhibition, but these tend to be mild and manageable with standard treatments.
- Patients with autoimmune disorders can respond to treatment at a rate similar to that of the general population, but they should be monitored closely for toxicities.
With regard to combination immunotherapy (eg, ipilimumab and nivolumab), we are generally hesitant to offer this treatment to patients with pre-existing autoimmune disease.[25] Again, a balanced yet frank discussion with the patient is indicated; this should include both consideration of consequences of immune flare and consideration of the patient’s cancer. Clearly, patients with severe autoimmune disease who are being treated with multiple biologic therapies or who have a history of life-threatening illness (eg, severe Crohn disease) will need a different approach than patients with minimally symptomatic autoimmune disease (eg, mild cutaneous psoriasis). In addition, a patient with highly symptomatic, high-volume metastatic melanoma may need a more aggressive approach than a patient with low-volume, asymptomatic disease. Newer immunotherapy combinations (eg, indoleamine 2,3-dioxygenase and PD-1 inhibitors) have yet to be tested in this setting.
Conclusions and Future Directions
Immune checkpoint inhibitors are transformative therapies that may produce sustained clinical benefits for responding patients. Understanding the interplay between pre-existing autoimmune disease and immunotherapy toxicities represents an important next step in efforts to extend the benefits of these therapies to additional patients. At this time, retrospective data largely suggest that patients with autoimmune disease can benefit from immunotherapy and experience tolerable toxicities that are manageable with immunosuppressive regimens. However, close clinical monitoring and multidisciplinary care are essential to the safe management of these patients. An ongoing prospective trial (ClinicalTrials.gov identifier: NCT02156804) is including a cohort of patients with autoimmune disease; this study should yield additional insights. In addition, the ongoing effort to understand immune checkpoint inhibitor toxicities at a molecular level may shed light on these questions.
Financial Disclosure:Dr. Johnson serves on advisory boards for Array Biopharma, Bristol-Myers Squibb, Incyte, Merck, Novartis, and Navigate BP; and he receives research funding from Bristol-Myers Squibb and Incyte. Drs. Beckermann and Wang have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. Postow MA. Managing immune checkpoint-blocking antibody side effects. Am Soc Clin Oncol Educ Book. 2015:76-83.
2. Wang DY, Johnson DB, Davis EJ. Toxicities associated with PD-1/PD-L1 blockade. Cancer J. 2018;24:36-40.
3. Le Burel S, Champiat S, Mateus C, et al. Prevalence of immune-related systemic adverse events in patients treated with anti-programmed cell death 1/anti-programmed cell death-ligand 1 agents: a single-centre pharmacovigilance database analysis. Eur J Cancer. 2017;82:34-44.
4. Le Burel S, Champiat S, Routier E, et al. Onset of connective tissue disease following anti-PD1/PD-L1 cancer immunotherapy. Ann Rheum Dis. 2018;77:468-70.
5. Johnson DB, Balko JM, Compton ML, et al. Fulminant myocarditis with combination immune checkpoint blockade. N Engl J Med. 2016;375:1749-55.
6. Gonzalez RS, Salaria SN, Bohannon CD, et al. PD-1 inhibitor gastroenterocolitis: case series and appraisal of ‘immunomodulatory gastroenterocolitis’. Histopathology. 2017;70:558-67.
7. Iwama S, De Remigis A, Callahan MK, et al. Pituitary expression of CTLA-4 mediates hypophysitis secondary to administration of CTLA-4 blocking antibody. Sci Transl Med. 2014;6:230ra45.
8. Donia M, Pedersen M, Svane IM. Cancer immunotherapy in patients with preexisting autoimmune disorders. Semin Immunopathol. 2017;39:333-7.
9. Tivol EA, Borriello F, Schweitzer AN, et al. Loss of CTLA-4 leads to massive lymphoproliferation and fatal multiorgan tissue destruction, revealing a critical negative regulatory role of CTLA-4. Immunity. 1995;3:541-7.
10. Wang J, Okazaki IM, Yoshida T, et al. PD-1 deficiency results in the development of fatal myocarditis in MRL mice. Int Immunol. 2010;22:443-52.
11. Nishimura H, Okazaki T, Tanaka Y, et al. Autoimmune dilated cardiomyopathy in PD-1 receptor-deficient mice. Science. 2001;291:319-22.
12. Kyi C, Carvajal RD, Wolchok JD, Postow MA. Ipilimumab in patients with melanoma and autoimmune disease. J Immunother Cancer. 2014;2:35.
13. Bostwick AD, Salama AK, Hanks BA. Rapid complete response of metastatic melanoma in a patient undergoing ipilimumab immunotherapy in the setting of active ulcerative colitis. J Immunother Cancer. 2015;3:19.
14. Johnson DB, Sullivan RJ, Ott PA, et al. Ipilimumab therapy in patients with advanced melanoma and preexisting autoimmune disorders. JAMA Oncol. 2016;2:234-40.
15. Lee B, Wong A, Kee D, et al. The use of ipilimumab in patients with rheumatoid arthritis and metastatic melanoma. Ann Oncol. 2016;27:1174-7.
16. Khan SA, Pruitt SL, Xuan L, Gerber DE. Prevalence of autoimmune disease among patients with lung cancer: implications for immunotherapy treatment options. JAMA Oncol. 2016;2:1507-8.
17. Weber JS, D’Angelo SP, Minor D, et al. Nivolumab versus chemotherapy in patients with advanced melanoma who progressed after anti-CTLA-4 treatment (CheckMate 037): a randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2015;16:375-84.
18. Menzies AM, Johnson DB, Ramanujam S, et al. Anti-PD-1 therapy in patients with advanced melanoma and preexisting autoimmune disorders or major toxicity with ipilimumab. Ann Oncol. 2016;28:368-76.
19. Bender C, Dimitrakopoulou-Strauss A, Enk A, Hassel JC. Safety of the PD-1 antibody pembrolizumab in patients with high-grade adverse events under ipilimumab treatment. Ann Oncol. 2016;27:1353-4.
20. Pollack MH, Betof A, Dearden H, et al. Safety of resuming anti-PD-1 in patients with immune-related adverse events (irAEs) during combined anti-CTLA-4 and anti-PD1 in metastatic melanoma. Ann Oncol. 2018;29:250-5.
21. Gutzmer R, Koop A, Meier F, et al. Programmed cell death protein-1 (PD-1) inhibitor therapy in patients with advanced melanoma and preexisting autoimmunity or ipilimumab-triggered autoimmunity. Eur J Cancer. 2017;75:24-32.
22. Danlos FX, Voisin AL, Dyevre V, et al. Safety and efficacy of anti-programmed death 1 antibodies in patients with cancer and pre-existing autoimmune or inflammatory disease. Eur J Cancer. 2018;91:21-9.
23. Abdel-Wahab N, Shah M, Lopez-Olivo MA, Suarez-Almazor ME. Use of immune checkpoint inhibitors in the treatment of patients with cancer and preexisting autoimmune disease: a systematic review. Ann Intern Med. 2018;168:121-30.
24. Cooper DS, Meriggioli MN, Bonomi PD, Malik R. Severe exacerbation of myasthenia gravis associated with checkpoint inhibitor immunotherapy. J Neuromuscul Dis. 2017;4:169-73.
25. Johnson DB, Sullivan RJ, Menzies AM. Immune checkpoint inhibitors in challenging populations. Cancer. 2017;123:1904-11.