Survivorship care is “a distinct phase of care for cancer survivors that includes four components: (1) prevention and detection of new cancer or recurrent cancer; (2) surveillance for cancer spread, recurrence, or second cancers; (3) intervention for consequences of cancer and its treatment; and (4) coordination between specialists and primary care providers to ensure that all of the survivor’s health needs are met.”[1] To promote the fourth component, coordination between specialists and primary care providers, the Institute of Medicine’s seminal 2006 report, “From Cancer Patient to Cancer Survivor: Lost in Transition” recommended-and the American College of Surgeons Commission on Cancer (CoC) requires-the development and delivery of survivorship care plans (SCPs) for all patients completing active treatment (Standard 3.3).[1,2] Standard 3.3 stipulates that “the cancer care committee develops and implements a process to disseminate a comprehensive care summary & follow-up plan to patients with cancer completing cancer treatment.”[2]
SCP development involves compiling a treatment summary and follow-up care plan; delivery involves providing a copy of the SCP to the patient and his or her primary care provider. Barriers to implementation of these recommendations include lack of agreed-upon standards for survivorship care; excessive time to prepare the SCP; perceived and actual shortage of oncology practitioners assigned to complete and deliver the SCP; the number of tumor types, each of which requires its own unique care plan; volume of patients; and lack of systems to facilitate this process.[3-6] In our large academic medical center, which sees about 5,000 new cancer patients per year within 11 disease groups, the Director of Cancer Survivorship was charged with implementing a process that would overcome these barriers and fulfill the CoC requirement. We were provided with an opportunity to develop and implement SCPs for adults completing cancer treatment with curative intent within our new electronic health record, Epic@UNC, using a systematic Lean Six Sigma approach.
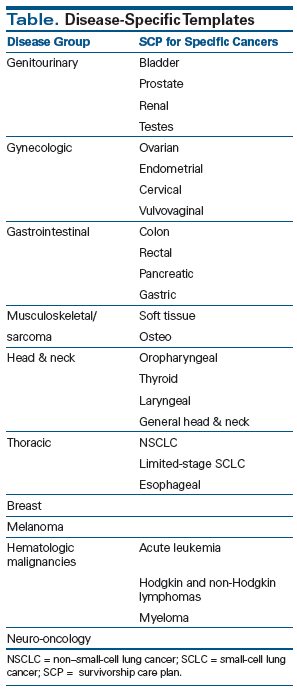
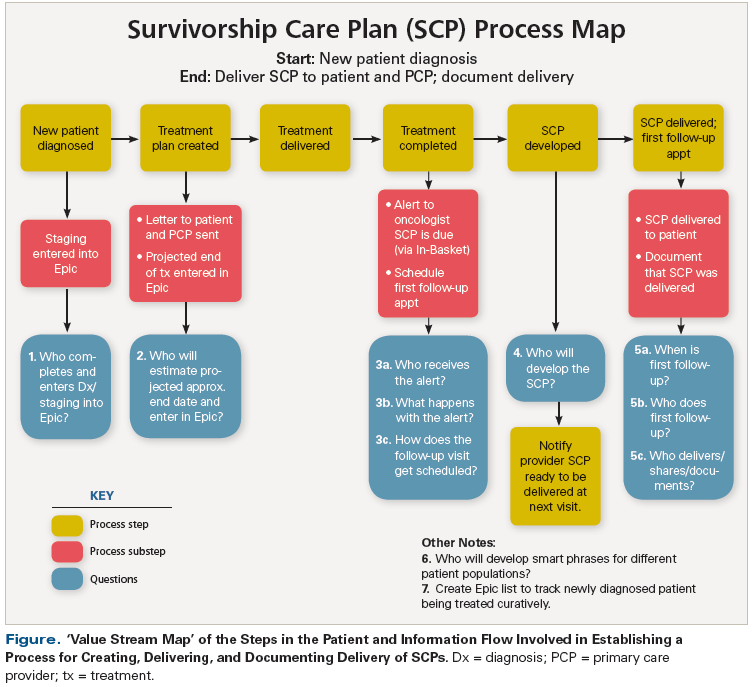
This process improvement method provides “a set of concepts, principles, and tools used to create and deliver the most value from the customer’s perspective while consuming the fewest resources”.[7,8] Express Workout is a Lean tool used for intense team problem solving; it is a tool that emphasizes speed, with the team identifying countermeasures and creating action plans to address barriers to optimal performance in a short period of time. Value stream mapping (VSM) was used to develop action plans for the delivery of SCPs within each disease group (Table). VSM provided a simple diagram of every step in the patient and information flow that was needed to complete each task in the process (eg, create the SCP). Specifically, VSM used visual representation to display the patient path and information flow from the beginning to the end of the process (Figure). It helped people understand how the process was supposed to work, helped them reach agreement on how well the process was actually working, helped uncover inefficiencies and problems with flow in the value stream, and helped people reach agreement on what changes needed to be made to effect improvements. We used VSM to define the steps needed to develop and deliver SCPs for all patients, since an SCP process did not exist.
We initially had Epic create the generic American Society of Clinical Oncology (ASCO) template content, modifying the look and feel to meet the specific needs of our institution (Epic@UNC). This was occurring at the same time that the national Epic organization was working with other users to anticipate the CoC Standard 3.3 and making this template available to other institutions.
We identified a physician in each disease group to champion SCP development and delivery within the group. This champion also appointed a disease group team leader (nurse practitioner or navigator) to be the point person who would oversee communication between his or her group and study staff for this project and who would help identify multidisciplinary groups of physicians, nurse practitioners, nurse navigators, and Patient and Family Advisory Board members from that disease group.
We met with each disease team to identify which cancers had enough volume to warrant creation of a standardized SCP template, then create a process for identifying eligible patients, track when these patients would complete treatment with curative intent, identify who would develop the SCP, and identify who would deliver the SCP to the patient and ensure that copies were also delivered to the primary care provider of record. Two groups (genitourinary and gynecology), actively led by their disease group team leaders, volunteered to be “early adopters” who would work with this process first. This was important, as they needed to contribute in an iterative manner to help develop the optimum way to create and deliver SCPs. We then identified one cancer in each of the disease groups (bladder and cervical, respectively) and asked the disease group to create “smart phrases” for each section of the template (including symptoms, surveillance, and possible late and long-term effects) that could then be inserted into the generic template. Smart phrases are created when the same statement may be needed multiple times (eg, statement about common side effects or the delivery of the document); they can be pulled into a document from an existing list.
KEY POINTS
Implementing Survivorship Care Plans Within an Electronic Health Record
- Implementing a process for the development and delivery of survivorship care plans (SCPs) requires multiple Plan-Do-Check-Act cycles involving key stakeholders.
- Creating the semi-automated SCP within an electronic health record is only one component of this process.
- Other issues that need to be addressed include creating systems for identifying eligible patients, knowing when the treatment ends, creating the SCP, determining when to deliver the SCP to the patient and relevant providers, and creating reporting functions to track use.
Teams used Plan-Do-Check-Act (PDCA) cycles, an iterative process, to facilitate continuous quality improvement, and to test the effectiveness of the SCPs for patients and providers, using specifically designed evaluation surveys that included quantitative data as well as qualitative data on patient and provider satisfaction. After a few PDCA cycles, based on feedback from our early adopters-and by observing them create SCPs-we realized that using smart phrases in a generic template was too time-consuming (taking about 20 minutes) and cumbersome (requiring at least three smart phrases per disease). As a result, we decided to create disease-specific care plans that included all of this information for the higher-volume cancers (see Table), and then use the generic ASCO template for others. This approach would minimize the amount of content to add and therefore take less time to complete. The process evolved into the following:
1. The disease group was given an Epic@UNC-formatted SCP draft template in a Microsoft Word document to adapt for each specific cancer, reflecting the group’s standards. They also discussed the processes for identifying patients, and then for tracking when patients would end treatment and when SCPs had been delivered to eligible patients ending curative treatment. Each group started by developing an SCP template for one cancer; once that went into production in Epic, other SCP templates were created, incorporating lessons learned from the first template.
2. The SCP template was then submitted to the Epic@UNC team for creation; a draft was validated by the disease group team before going into production. Each SCP template was mapped to the correct ICD-9/10 codes for that cancer, so that the right template attached to the correct diagnosis.
3. Once the SCP template became available in Epic@UNC, it was piloted in a few patients to identify any changes needed from either the provider’s or the patient’s perspective. If it was determined that changes were needed, a change request was submitted to Epic@UNC.
4. Once the changes were made, the SCP process was then presented to the entire tumor group during a tumor board meeting at which the team discussed their pilot experiences. At that time, the disease group was then expected to begin SCP implementation as adopted by their group, with the champion and project leader serving as contacts for issues that might arise. The disease teams met regularly after the SCP template was launched to reevaluate and monitor its effectiveness and patient satisfaction.
Increased autocompletion of the SCP decreased the time to completion from about 20 minutes to about 5 minutes. This time should continue to decrease as more fields within the SCP (eg, diagnosis, stage) are able to be autopopulated after future software updates. The steps required to create an SCP dropped from nine steps to four; access to the SCP from within a patient’s problem list (which is centrally located on the home page of the patient’s medical record in Epic@UNC) was also made easier-no longer requiring five clicks into the medical record to find it. The “tip sheet” of instructions for Epic-based SCP creation, which provided step-by-step directions for completing the creation of an SCP, went from five pages to two. Additionally, we are working to have a report function created within Epic that will give tumor groups feedback on the number of patients eligible for an SCP and the number who have actually received the SCP.
Ongoing communication between the various disease teams and the Epic developers has been necessary to facilitate this process. The Director of Survivorship provided updates at the Hospital’s Committee on Cancer quarterly meeting. Our goal is to increase SCP use for more patients as we address the CoC Standard 3.3 metrics. We need to evaluate the effect that receipt of an SCP has on outcomes such as adherence to surveillance recommendations. We are committed to using the SCP process to support collaboration and communication with, and education of, our survivors and their primary care providers, but we expect that we will continually revise this process until it becomes a standard of cancer care.[9-11]
Acknowledgments: This project was funded by the University of North Carolina Institute for Healthcare Quality Improvement. We would like to thank Dr. Michael Pignone and Laura Brown for their guidance and support of this project. We would also like to thank the genitourinary and gynecology teams for being early adopters for this project.
Financial Disclosure:Dr. Mayer serves as an advisor to CareVive Systems. The other authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. Hewitt M, Greenfield S, Stovall E, eds. From cancer patient to cancer survivor: lost in transition. Washington, DC: The National Academies Press; 2005.
2. American College of Surgeons. Cancer program standards 2012, Version 1.2.1: Ensuring patient-centered care. 2012.
3. Mayer DK, Gerstel A, Walton A, et al. Implementing survivorship care plans (SCP) for colon cancer survivors in a comprehensive cancer center. Oncol Nurs Forum. 2014;41:266-73.
4. Birken SA, Deal AM, Mayer DK, Weiner BJ. Determinants of survivorship care plan use in United States cancer programs. J Cancer Educ. 06 Apr 2014. [Epub ahead of print]
5. Birken SA, Deal AM, Mayer DK, Weiner BJ. Following through: the consistency of survivorship care plan use in United States cancer programs. J Cancer Educ. 2014;29:689-97.
6. Birken S, Deal A, Mayer DK, Weiner B. Prevalence and barriers to survivorship care plan use in United States cancer programs. J Cancer Educ. 2014 Apr 6. [Epub ahead of print]
7. Lean Enterprise Institute. http://www.lean.org/. Accessed November 24, 2015.
8. Varkey P, Reller MK, Resar RK. Basics of quality improvement in health care. Mayo Clin Proc. 2007;82:735-9.
9. Dunn R, Crowley S, Janz N, et al. Impact of a transition visit on addressing quality of life and readiness to assume greater self-management among breast cancer survivors. https://www.gem-beta.org/Public/MeasureDetail.aspx?cat=2&mid=1391&tab=6. Accessed November 17, 2015.
10. Glasgow R, Rabin B. New and future directions in implementation science: some things to consider in your next grant or two. 13 Jan 2014. http://www.youtube.com/watch?v=ulUQ2NWtfN8. Accessed November 17, 2015.
11. Malin J, Sayers E, Jefford M. What is quality health care for cancer survivors? In: Feuerstein M, Ganz PA, eds. Health services for cancer survivors. New York, NY: Springer; 2011. p. 27.