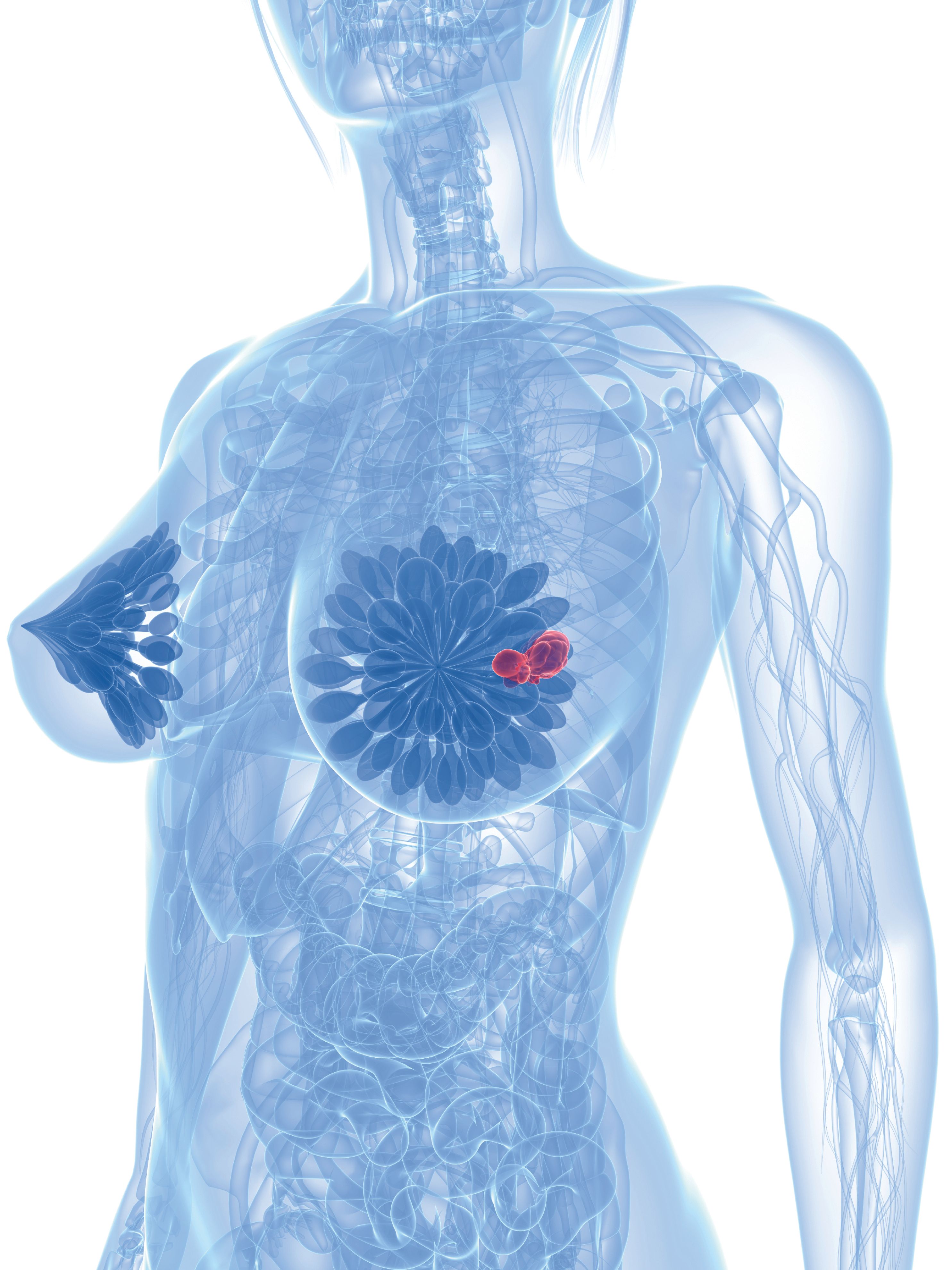
Inavolisib Combo Meets OS End Point in PIK3CA+ Metastatic Breast Cancer
The phase 3 INAVO120 trial reported statistically significant OS results in patients with PIK3CA-mutant, locally advanced or metastatic breast cancer.
The phase 3 INAVO120 trial reported statistically significant OS results in patients with PIK3CA-mutant, locally advanced or metastatic breast cancer.
The combination of inavolisib (Itovebi) with palbociclib (Ibrance) and fulvestrant (Faslodex) produced positive topline results, meeting the key secondary end point of overall survival (OS) in the phase 3 INAVO120 trial (NCT04191499), in the treatment of patients with PIK3CA-mutated, hormone receptor (HR)–positive, HER2-negative, endocrine-resistant, locally advanced or metastatic breast cancer, according to a press release from the developer, Roche.1
In October 2024, this drug combination was approved in patients with PIK3CA-mutated, HR–positive, HER2-negative, endocrine-resistant, locally advanced or metastatic breast cancer after recurrence on or after adjuvant endocrine therapy based on findings from the INAVO210 trial.2 Additionally, the INAVO120 trial was previously reported to have met its primary end point of progression-free survival (PFS).3
The inavolisib with palbociclib and fulvestrant regimen elicited statistically significant and clinically meaningful OS results, improving over outcomes with palbociclib and fulvestrant alone. Full OS results from the trial will be shared at an upcoming medical meeting.
"The INAVO120 OS results show that the [inavolisib]-based regimen not only delayed disease progression, but also helped people with advanced HR–positive, PIK3CA-mutated breast cancer live longer,” Levi Garraway, MD, PhD, chief medical officer and head of Global Product Development at Roche, said in the press release.1 “These findings underscore our ambition to improve survival rates for people with breast cancer. The [inavolisib]-based regimen has the potential to become the new standard of care for these patients.”
Although OS data was not mature at the time of the interim analysis, at 6, 12, and 18 months, the probability of survival was 97.3%, 85.9%, and 73.7%, respectively, in the experimental group, and 89.9%, 74.9%, and 67.5%, respectively, in the control group. The stratified HR for death was 0.64 (95% CI, 0.43-0.97; P = .03).
The randomized, double-blind, placebo-controlled INAVO120 study enrolled a total of 325 patients who were randomly assigned to the experimental group (inavolisib, palbociclib, and fulvestrant) or the control group (placebo, palbociclib, and fulvestrant). Patients received either 9 mg of oral inavolisib once daily during each 2-day cycle or matching placebo once daily, and both groups received 125 mg of palbociclib once daily on days 1 to 21 every cycle and 500 mg of fulvestrant intramuscularly on days 1 and 15 for the first cycle, then once every every 28 days.
The overall median age of patients was 54.0 (range, 27-79), 98.2% of patients were female, 63.4% had an ECOG performance status of 0, and 60.0% of patients were postmenopausal.
Additionally, 51.4% of patients had 3 or more organs with metastases; the most common sites of metastases were viscera (80.0%), liver (51.7%), lung (40.6%), and bone only (3.4%). Estrogen receptor–positive and progesterone receptor–positive status was observed in 69.5% of patients, and 65.5% had secondary resistance to endocrine therapy.
Previous neoadjuvant or adjuvant chemotherapy and endocrine therapy were observed in 82.8% and 99.4% of patients, respectively. The most common endocrine therapies were tamoxifen only (47.7%), aromatase inhibitor only (40.3%), and aromatase inhibitor and tamoxifen (11.4%).
At a median follow-up of 21.3 months in the experimental group and 21.5 months in the control group, median PFS was 15.0 months (95% CI, 11.3-20.5) vs 7.3 months (95% CI, 5.6-9.3), respectively (HR, 0.43; 95% CI, 0.32-0.59; P <.001).
Objective responses occurred in 58.4% of the experimental group and 25.0% of the control group (difference, 33.4%; 95% CI, 23.3%-43.5%), and median duration of response was 18.4 months vs 9.6 months, respectively (HR, 0.57; 95% CI, 0.33-0.99).
Regarding safety, at least 1 adverse event (AE) occurred in 98.8% of the experimental group and 100% of the placebo group. The most common AEs of any grade were neutropenia (88.9% vs 90.7%, respectively), hyperglycemia (58.6% vs 8.6%), stomatitis and mucosal inflammation (51.2% vs 26.5%), and thrombocytopenia (48.1% vs 45.1%). Of grade 3 and 4 toxicities, the most common AEs were neutropenia (80.2% vs 78.4%, respectively), leukopenia (6.8% vs 10.5%), thrombocytopenia (14.2% vs 4.3%), and anemia (6.2% vs 1.9%).
AEs led to discontinuation of any trial drug in 6.8% of the experimental group and 0.6% of the control group, and dose reduction occurred in 14.2% and 3.1%, respectively. No deaths were associated with the study treatment.
References
- Roche’s Itovebi demonstrated statistically significant and clinically meaningful overall survival benefit in a certain type of HR-positive advanced breast cancer. News release. Roche. January 27, 2025. Accessed January 28, 2025. https://tinyurl.com/3cyk734s
- FDA approves inavolisib with palbociclib and fulvestrant for endocrine-resistant, PIK3CA-mutated, HR-positive, HER2-negative, advanced breast cancer. News release. FDA. October 10, 2024. Accessed January 28, 2025. https://tinyurl.com/mr4xknj8
- Turner NC, Im S-A, Saura C, et al. Inavolisib-based therapy in PIK3CA-mutated advanced breast cancer. N Engl J Med. 2024;391(17):1584-1596. doi:10.1056/NEJMoa2404625
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.