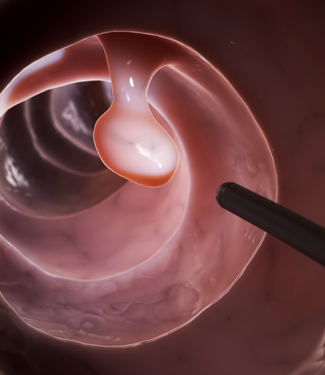
Increased Colorectal Cancer Screening May Decrease Incidence, Mortality
If US colorectal cancer screening is increased to 80% by 2018, a new study predicts a decrease in both cancer incidence and mortality within 20 years.
Image © Sebastian Kaulitzki/Shutterstock.com
If the healthcare community is able to meet the National Colorectal Cancer Roundtable’s goal of increasing uptake of colorectal cancer screening in the United States to 80% by 2018, a new study estimates that 280,000 new cancer cases and 200,000 cancer deaths could be averted within 20 years.
According to the study published in the journal Cancer, only 58% of US adults aged 50 to 75 years received guideline-recommended colorectal screening in 2013. The National Colorectal Cancer Roundtable, a national coalition of public, private, and voluntary organizations, recently announced an effort to increase this rate of screening to 80%, a 22% increase, by 2018.
In this study, Reinier G. S. Meester, MS, of the department of public health at Erasmus MC University Medical Center in Rotterdam, Netherlands, and colleagues used modeling to try to estimate the possible benefits of achieving this increased screening goal.
To get these estimates, Meester and colleagues simulated the 1980 through 2030 US population of individuals aged 50 to 100 years, including historical screening rates based on National Health Interview Survey data for 1987 to 2013. They then compared the effects of increasing the approximately 58% current screening rate to 80% by 2018 with a scenario where screening remained constant.
Assuming that screening rates were to otherwise stay constant between 2013 and 2030, the rate of colorectal cancer incidence per 100,000 people per year would increase from 137 in the first year to 149 in 2030, due to population aging. However, if during this same time period the rate of screening increased by 22%, the researchers found that the incidence rates would decrease from 164 per 100,000 in 2014 to 117 per 100,000 in 2030.
“Compared with a scenario of constant colorectal cancer screening levels, the goal of ‘80% by 2018’ would initially increase colorectal cancer incidence rates by 20% in 2014 because of the early detection of colorectal cancer among previously unscreened individuals, but subsequently decrease the incidence rates by 17% by 2020 and by 22% by 2030,” the researchers wrote.
Under these assumptions, 43,000 cases of colorectal cancer would be averted each year by 2030 for a total of 277,000 cases averted from 2013 to 2030.
According to the researchers, this increased screening rate would have immediate effects on colorectal cancer mortality. With a constant rate of screening, colorectal cancer mortality would be expected to increase from 44 per 100,000 in 2014 to 48 per 100,000 in 2030; however, with increased screening this rate would decline from 43 to 32 per 100,000.
“Thus, the relative effect of the ‘80% by 2018’ goal would be a 1% decrease in the colorectal cancer mortality rate by 2014, a decrease of 19% in 2020, and a decrease of 33% in 2030,” the researchers wrote.
The researchers acknowledged that this study only looked at increasing screening by expanding screening to include previously unscreened adults. However, screening could also be expanded by reducing the numbers of adults screened, but not according to screening recommendations, which is estimated to be about 7.4% of people who are screened.
“Thus, in a strategy of encouraging both higher guideline adherence in previously screened individuals and the participation of previously unscreened individuals, the former approach could contribute approximately one-third (7.4%) to the overall targeted increase of 22% in screening rates,” the researchers wrote. “This may lead to a somewhat lower public health impact for the ‘80% by 2018’ goal than we found because the impact of screening is lower in previously screened individuals compared with unscreened individuals.”