At Increased Cost, Robotic Partial Nephrectomy Improves Kidney Cancer Outcomes
A study found that robotic partial nephrectomy to remove kidney cancer tumors resulted in better outcomes, but also had significantly higher hospital charges. The data were presented at the annual meeting of the American Urological Association.
The use of robotic partial nephrectomy to remove kidney cancer tumors has increased in recent years, becoming more commonly used than open or laparoscopic partial nephrectomy and resulting in better outcomes. However, data from a study presented at the American Urological Association Annual Meeting also showed that the procedure is associated with significantly higher hospital charges as well.
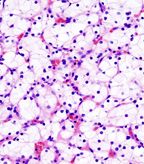
Histopathologic image of clear cell carcinoma of the kidney; nephrectomy specimen; source: KGH, Wikimedia Commons
“This is the first analysis of robotic kidney surgery within the United States using a large federally held database and is therefore representative of broad practices,” said Khurshid R. Ghani, MD, of Vattikuti Urology Institute. “We have shown that there has been a dramatic uptake of robotic partial nephrectomy throughout the country, and it is now more popular than the laparoscopic approach.”
Although the use of partial nephrectomy has been increasing, research had not yet shown conclusively that it is a better operation than the traditional open or laparoscopic approaches.
Dr. Ghani and colleagues used data from the Nationwide Inpatient Sample from October 2008 to December 2010 to identify all patients who underwent open partial nephrectomy, laparoscopic partial nephrectomy, or robotic partial nephrectomy. Data were examined for practice patterns and perioperative outcomes.
Specifically, of 38,064 partial nephrectomies during the study period, 66.9% were open, 9.2% were laparoscopic, and 23.9% were robotic. In 2010, the relative increase in utilization of robotic partial nephrectomy was 45.4%, compared with 7.9% for open and 6.1% for laparoscopic.
“More importantly, compared to open or laparoscopic partial nephrectomy, robotic partial nephrectomy had much lower complications,” Dr. Ghani told Cancer Network.
Patients who underwent either minimally invasive procedure had significantly reduced odds of receiving a blood transfusion (robotic, OR = 0.56, P < .001; laparoscopic, OR = 0.68, P = .016), postoperative complication (robotic, OR = 0.63, P < .001; laparoscopic OR = 0.78, P < .009), or experience a prolonged length of stay (robotic, OR = 0.27, P < .001; laparoscopic, OR = 0.41, P < .001).
In addition, a robotic procedure resulted in a reduced risk for intraoperative complications.
However, robotic kidney surgery costs more than the other two operations.
“It is likely that robotic kidney surgery will now become the predominant method to remove kidney tumors in the United States,” Dr. Ghani said. “Recently, there has been some negative press coverage on robotic kidney surgery, especially after a large study reported on outcomes after robotic hysterectomy. Our study shows robotic kidney surgery is safe and comparable, if not superior.”