Intensity-Modulated Radiation Therapy Offers Greater Coverage, Fewer Toxicities
Adding a third dimension to the therapeutic field and reversing treatment planning may provide safer and more effective dose delivery, according to recent studies discussed at the Miami Breast Cancer Conference.
Adding a third dimension to the therapeutic field and reversing treatment planning may provide safer and more effective dose delivery, according to recent studies discussed at the Miami Breast Cancer Conference.
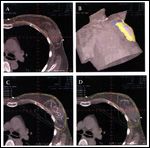
Images of forward planning IMRT in breast cancer patient
A relatively new technique, intensity-modulated radiation therapy (IMRT), builds on CT-based treatment planning, which was itself a significant advance over early two-dimensional techniques. With the help of sophisticated imaging, clinicians could "sculpt the radiation field and clearly delineate normal tissue," said Lori J. Pierce, MD, professor of radiation oncology at the University of Michigan School of Medicine in Ann Arbor.
"Then along came IMRT, another form of three-dimensional planning that allows even more degrees of freedom," added Dr. Pierce.
Rather than providing uniform intensities, IMRT uses computerized optimization to break up the field and conform doses to the size, shape, and location of the breast tumor. Intense radiation can reach targeted cancer cells with minimal exposure to healthy tissues.
The result is a "more colorful picture," said Dr. Pierce. "But does it actually translate into benefits for patients?"
She shared highlights from a growing body of evidence that suggests it just might, thanks not only to improved dose delivery but also to decreased acute and long-term toxicities.
A randomized study out of Canada, published in 2008 in the Journal of Clinical Oncology (DOI: 10.1200/ JCO.2007.15.2488), found that IMRT's more homogeneous distribution reduced the rate of moist desquamation compared to two-dimensional techniques (31% versus 48%, P = .002). The condition was linked with pain (P = .002) and a reduced quality of life (P = .003).
Another study published in Radiotherapy and Oncology in 2007 (doi:10.1016/ j.radonc.2006.12.008) found that standard two-dimensional radiation led to 1.7-fold more changes in the appearance of the breast after 5 years compared to IMRT (58% versus 40%, P = .0008). Patients treated with IMRT also experienced less palpable induration. The study did not demonstrate a benefit to quality of life with IMRT, however.
Further, Dr. Pierce pointed to a study presented at the 2009 San Antonio Breast Cancer Symposium (abstract 71), which found that IMRT led to better cosmetic results, including fewer skin changes, compared to two-dimensional radiation.
Missing from studies to-date is an evaluation of IMRT's impact on normal tissues. Dr. Pierce noted that ongoing trials, including a pilot study of her own at the University of Michigan, are addressing whether or not IMRT spares critical tissues of the heart and lung.
For some patients, she added, there might be equally effective techniques that are less complicated, time-intensive and costly. Do to the necessary manpower and equipment, IMRT can cost between 1.5 and 3 times more than non-IMRT techniques.
"The patients that are likely to derive the greatest benefit need to be better defined," Dr. Pierce said. "Patients differ, and so will their requirements for planning."