INTERIM Confirms 5-Year Efficacy of Intermittent Imatinib in CML
Long-term follow-up confirmed the previously reported result that intermittent administration of imatinib is safe and effective in CML patients.
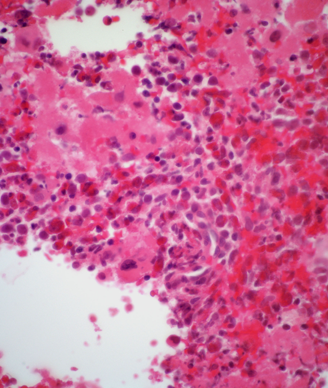
CML showing atypical lymphoid cells
Long-term follow-up confirmed the previously reported result that intermittent administration of imatinib is safe and effective in chronic myeloid leukemia (CML) patients. The INTERIM trial’s 5-year follow-up results were reported in December at the American Society of Hematology (ASH) Annual Meeting in San Francisco.
The phase II trial included 76 patients who were at least 65 years old, and all had a stable complete cytogenetic response (CCgR) lasting more than 2 years. The intermittent imatinib regimen was a 1 month on, 1 month off schedule. After 4 years of follow-up, 75% continued on the intermittent schedule, and those who had lost CCgR (17%) and major molecular response (MMR; 18%) resumed a continuous imatinib schedule. All of those patients regained CCgR and MMR within 3 to 12 months.
After the 5-year follow-up analysis, 45 of the initial 76 patients (59%) remained on the intermittent schedule. No patient lost CCgR between the 4- and 5-year time points, and nine additional patients lost MMR; again, all of those patients resumed normal scheduling of imatinib and subsequently regained the MMR. “Thus, at ≥ 5 years, the probability of maintaining CCgR is 80% (95% CI, 68%–87%) and the probability of maintaining the MMR is 61% (95% CI, 48%–71%),” wrote researchers led by Domenico Russo, MD, of the University of Brescia in Italy, in an abstract.
Six patients died since the start of the INTERIM trial, but none were related to CML progression; there were three cases of other non-hematological neoplasms, one stroke, one myocardial infarction, and one case of chronic obstructive pulmonary disease. The progression-free survival rate at ≥ 5 years was 94%.
“In summary, with a follow-up of ≥ 5 years, intermittent imatinib administration [was] confirmed to be safe, to produce a reversible increase of residual molecular disease in about one-third of patients, but not to affect the long-term outcome,” the researchers wrote.
There has been substantial interest in intermittent or other alternative scheduling of tyrosine kinase inhibitors in treatment for CML. The success of the drugs has been remarkable, but because of that success and the relative young age of many CML patients, many are forced to take the drugs for many years and even decades. This carries high financial burden, as well as increasing chances of non-compliance. Affirming the safety of intermittent scheduling could ease some of those concerns in CML patients.