JSKN003 Earns FDA Breakthrough Therapy Designation for HER2-Expressing PROC
Pooled analysis data from the phase 1 JSKN003-101 and phase 1/2 JSKN003-102 trials support the regulatory decision.
Patients with confirmed HER2 immunohistochemistry experienced an ORR of 72.2% and a DCR of 94.4%, with both CRs occurring in this patient subgroup.
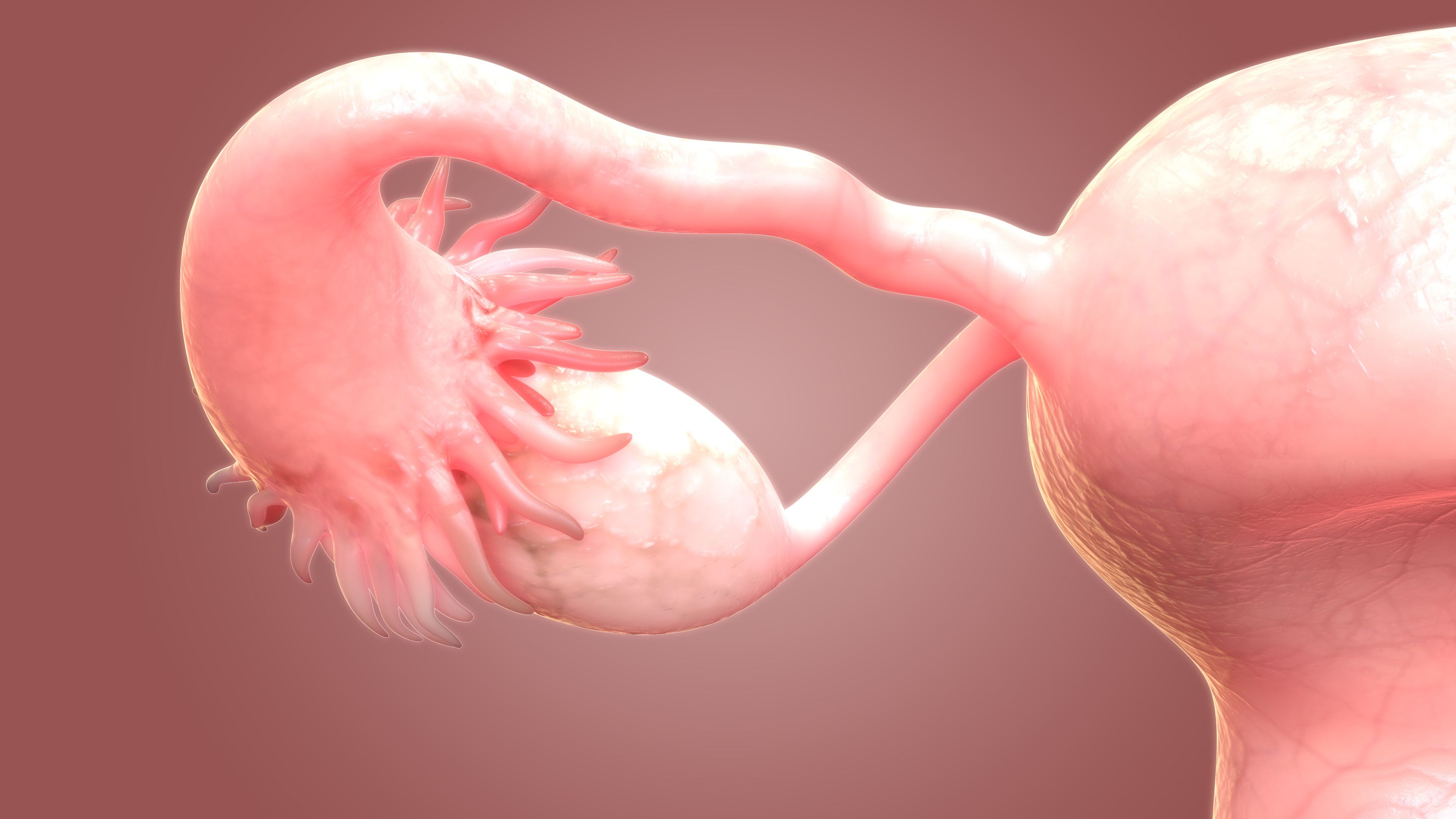
JSKN003, a biparatopic HER2-targeting antibody drug conjugate (ADC), has been granted breakthrough therapy designation by the FDA as a treatment for adult patients with advanced or metastatic HER2-expressing platinum-resistant recurrent epithelial ovarian cancer, primary peritoneal, or fallopian tube cancers (PROC) previously treated with bevacizumab (Avastin), according to a news release from the drug’s developer, Alphamab Oncology.1
Supporting the regulatory decision was a pooled analysis of the phase 1 JSKN003-101 (NCT05494918) and phase 1/2 JSKN003-102 trials (NCT05744427) presented at the 2025 American Society of Clinical Oncology (ASCO) Annual Meeting.2 The investigational agent was evaluated as a monotherapy across multiple dose levels from 4.2 to 8.4 mg/kg in both trials.
Findings from the pooled analysis revealed an objective response rate (ORR) of 63.0% (95% CI, 47.5%-76.8%) among 46 patients with PROC treated with JSKN003. Additionally, 2 patients (4.3%) had attained a complete response (CR), and 27 patients (58.7%) had experienced a partial response as best response after a median follow-up of 9.3 months. The disease control rate was 93.5% (95% CI, 82.1%-98.6%) for this group.
Moreover, the median progression-free survival (PFS) was 7.7 months (95% CI, 5.7-9.7). The median overall survival (OS) was not reached as of data cutoff, and the 9-month OS rate was 89.9% (95% CI, 75.0%-96.1%).
Patients with confirmed HER2 immunohistochemistry (IHC; n = 18) experienced an ORR of 72.2% (95% CI, 46.5%-90.3%) and a DCR of 94.4% (95% CI, 72.7%-99.9%), with both CRs occurring in this patient subgroup. The median PFS was 9.4 months (95% CI, 5.7-not evaluable [NE]), and the 9-month OS rate was 82.5% (95% CI, 54.9%-94.0%).
“Patients with PROC have limited treatment options, with non-platinum chemotherapy showing low response rates of 10% [to] 15%, short median PFS of 3 [to] 4 months, and short OS of 12 months,” study investigator Xiaohua Wu, MD, PhD, of the Department of Gynecologic Oncology at Fudan University Shanghai Cancer Center in Shanghai, China, wrote in the presentation with coinvestigators.2 “With extended follow-up, JSKN003 demonstrated robust PFS improvement in PROC, along with early signals of OS benefit.”
Those with PROC treated in the pooled analysis (n = 48) initially had tissue samples collected for central lab assessment of HER2 expression status. Most patients received the recommended phase 2 dose of 6.3 mg/kg (n = 40), with 2 patients receiving 4.2 or 5.2 mg/kg each, and 1 patient receiving 7.3 or 8.4 mg/kg each. Patients received treatment once every 3 weeks.
Among all patients included in the efficacy analysis (n = 46), the median age was 59.0 years (IQR, 53.0-63.0). A total of 84.8% of patients were Asian, 56.5% had an ECOG performance status of 1, and 91.3% had a tumor diagnosis of ovarian cancer. Most patients had a HER2 IHC of 0 (45.7%) or 1 (21.7%), a platinum-free interval of greater than 3 months (50.0%), and had received 3 or more lines of prior anti-cancer therapy (65.2%), including bevacizumab (Avastin; 80.4%) and PARP inhibition (63.0%).
In both trials, primary end points included the maximum tolerated dose and adverse effects (AEs)/dose-limiting toxicities.3,4 An additional primary end point in the phase 1/2 trial was ORR. Secondary end points in both trials included PFS and duration of response.
Treatment-related AEs (TRAEs) occurred in 95.7% of patients in the pooled analysis. Grade 3/4 TRAEs were observed in 19.6% of patients, and 13.0% experienced serious TRAEs. No TRAEs were fatal.
The most common any-grade TRAEs included anemia (39.1%), aspartate aminotransferase increases (39.1%), diarrhea (37.0%), nausea (37.0%), and asthenia (34.8%). The most common TRAEs of grades 3/4 included anemia (6.5%), lymphocyte count decreases (4.3%), asthenia, and platelet count decreases (2.2% each). Of note, interstitial lung disease events were reported in 5 (10.9%) patients and were grade 1 or 2 in severity.
The FDA previously granted fast track designation to JSKN003 in the same patient group in October 2025.5
References
- Alphamab Oncology announces biparatopic HER2-targeting ADC JSKN003 was granted breakthrough therapy designation by the FDA for the treatment of PROC. News release. Alphamab Oncology. December 20, 2025. Accessed December 22, 2025. https://shorturl.at/B3aDO
- Wu X, Chen Y, Rao Q, et al. JSKN003, a biparatopic anti-HER2 antibody drug conjugate (ADC), in the treatment of platinum-resistant ovarian cancer (PROC): Updated findings from two clinical trials. J Clin Oncol. 2025;43(suppl 16):107. doi: 10.1200/JCO.2025.43.16_suppl.5557
- First-in-human study in subjects with advanced or metastatic solid malignant tumors. ClinicalTrials.gov. Updated August 22, 2025. Accessed December 22, 2025. https://tinyurl.com/nzv8zszn
- Safety and tolerability of JSKN003 in Chinese subjects with advanced solid tumors. Updated September 15, 2025. Accessed December 22, 2025. https://tinyurl.com/mvdur8sm
- Alphamab Oncology announces biparatopic HER2-targeting ADC JSKN003 was granted fast track designation by FDA for the treatment of PROC. News release. Alphamab Oncology. October 27, 2025. Accessed December 22, 2025. https://tinyurl.com/5n87t26z