Kidney Condition Adds Morbidity in Cervical Cancer
Hydronephrosis is associated with substantial morbidity in patients with cervical cancer, and is potentially associated with poorer survival as well.
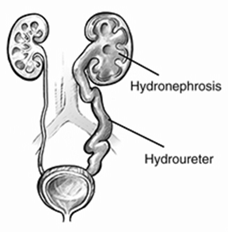
Hydronephrosis develops when a blockage in the renal collecting system results in distention of renal calyces.
Hydronephrosis is associated with substantial morbidity in patients with cervical cancer, and is potentially associated with poorer survival as well, according to a new study.
Hydronephrosis, essentially a swelling of the kidney, develops when a blockage in the renal collecting system results in distention of renal calyces. “Women with cervical cancer often develop this complication as a result of tumor or lymph node encroachment, inflammation, or scarring at the pelvic rim,” wrote study authors led by Aminah Jatoi, MD, of the Mayo Clinic in Rochester, Minnesota. Stent placement or urinary diversion procedures are often used as treatment for the complication.
Investigators undertook a study of morbidities associated with this condition due to a lack of research on the topic and its relative frequency in cervical cancer patients. Also, earlier work suggested worse survival in those with hydronephrosis, but those studies are old and may not reflect current practices and experience. In the new study, 279 patients with cervical cancer were included; 65 of those (23%) were diagnosed with hydronephrosis at some point during their disease course. Results were published online ahead of print on October 23 in Supportive Care in Cancer.
Univariate analyses found that cancer stage (III–IV vs I–II), non-surgical treatment of cancer, and tumor histology were significantly associated with hydronephrosis occurrence. Multivariate results were similar, though tumor histology was no longer significantly associated.
Seventeen patients with hydronephrosis experienced “notable morbidity.” This included pain, urinary tract infections, nausea and vomiting, renal failure, and urinary tract bleeding. Seven patients experienced more than one of these types of morbidity.
Survival data was available for 278 of the patients, and 221 were still alive after a median follow-up of 1.5 years. The 3-year survival rate was 37% in patients with hydronephrosis and 74% in those without it, for a hazard ratio of 4 (95% CI, 1.75–8.01; P = .0021). Adjustments for patient age at diagnosis, tumor stage, nonsurgical cancer treatment, and tumor histology rendered this association non-significant, however (P = .2097). But when investigators conducted landmark multivariate analyses, hydronephrosis was associated with worse survival from 9 to 18 months post-cancer diagnosis.
The seriousness of the complication suggests there is room to improve daily clinical practice for the treatment of cervical cancer patients. “We conclude that patients might benefit from better counseling related to this morbidity,” Jatoi said in an email. “Second, we think that further research in this area is warranted; overall there has not been a great deal of research undertaken on the topic.” Key questions include a better understanding of the prognostic effect of hydronephrosis, as well as how to reduce it and improve survival in these patients.