KRAS-Mutated Lung Adenocarcinomas Yield Shorter Overall Survival
The presence of a mutation in the KRAS gene in patients with advanced lung adenocarcinomas was associated with significantly shorter overall survival than patients without the mutation, according to a new study.
The presence of a mutation in the KRAS gene in patients with advanced lung adenocarcinomas was associated with significantly shorter overall survival when compared to patients without the mutation, according to a new study. The large single-center analysis confirmed previous findings that mutations in the epidermal growth factor receptor (EGFR), meanwhile, are associated with longer overall survival in this patient population.
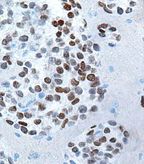
High magnification micrograph of a primary lung adenocarcinoma showing nuclear staining with a TTF-1 immunostain; source: Nephron, Wikimedia Commons
EGFR mutations are present in 10% to 15% of US patients diagnosed with advanced lung adenocarcinomas, while KRAS mutated patients make up about 30% of patients. Patients with EGFR mutations have been shown to have longer progression-free survival compared to those with EGFR wild-type tumors, and they also respond well to targeted tyrosine kinase inhibitors such as erlotinib (Tarceva) and gefitinib (Iressa). Meanwhile, “the natural history of patients with KRAS mutations has been difficult to understand historically because the numbers of patients studied was small and analyses retrospective,” said study lead author Melissa L. Johnson, MD, of the Robert H. Lurie Comprehensive Cancer Center at Northwestern University in Chicago, in an email to Cancer Network. The study was published online ahead of print in July in Cancer.
The study included 1,036 patients with stage IV lung adenocarcinoma evaluated at the Memorial Sloan-Kettering Cancer Center between 2002 and 2009. Of these, 275 tumors (27%) had EGFR mutations and 241 tumors (23%) had KRAS mutations. The remaining 520 tumors (50%) were wild-type for both EGFR and KRAS. Thirty-three percent of the cohort were never-smokers; most of these were EGFR-positive patients, with never-smokers making up 60% of that group.
In a multivariate analysis, EGFR mutations were associated with a longer overall survival than those without EGFR mutations (hazard ratio [HR], 0.6; P < .001). In contrast, patients with KRAS mutations had shorter overall survival when compared to those with wild-type KRAS (HR, 1.21; P = .048).
The authors noted that the study confirmed previously determined prognostic value for factors including sex, age, performance status, and smoking status, as well as EGFR mutations. “In this, the largest collection of patients to date with advanced lung adenocarcinomas and KRAS mutations from one institution, we also demonstrate that the presence of a KRAS mutation is an independent factor associated with shorter survival,” they wrote.
Importantly, that association with shorter overall survival persisted in spite of the finding that KRAS-mutated patients were equally likely as wild-type KRAS and EGFR-mutated patients to have received platinum-based chemotherapy and bevacizumab (Avastin). That similarity in treatment suggests that the poorer survival with KRAS mutations is linked to inherent differences in tumor biology rather than in how the patients are managed. Not surprisingly, patients with EGFR mutations were significantly more likely than others to have received EGFR-TKIs (97% vs 30%; P < .001).
Among the primary implications of this finding, Dr. Johnson said, is that KRAS-mutated tumors should be treated as having a distinct clinical course from other lung adenocarcinomas. Thus, they “should be evaluated separately in clinical trials,” she said. The authors wrote that KRAS testing should be done along with EGFR and EML4-ALK mutation testing to prospectively identify these patients in the clinic.