Latest PARSPORT Results Confirm: IMRT Greatly Reduces Treatment Effects in Head and Neck Cancer
Two-year results from the largest randomized trial of IMRT in head and neck cancer confirm that it dramatically reduces the risk of dysphagia and xerostomia. The study was too small to establish a survival advantage, although the results are encouraging.
Two-year results from PARSPORT, the first randomized trial to compare intensity-modulated radiotherapy (IMRT) with conventional radiotherapy for head and neck cancer, appeared last week in Lancet Oncology. They confirm earlier findings from PARSPORT and from single-center retrospective trialsthat suggested that IMRT dramatically reduces the risk of dysphagia and xerostomia among patients with head and neck cancer.
The UK-based multicenter PARSPORT was limited to patients with squamous cell carcinoma, the most common form of head and neck cancer. But the authors contend that the results should apply to by analogy to "all other head and neck tumours for which conventional radiotherapy is used," because smaller trials have shown similar results for nasopharyngeal cancer.
The largest randomized trial of IMRT in head and neck cancer and the only one to involve squamous cell carcinoma, PARSPORT randomized 94 patients to receive either parotid-sparing IMRT or conventional radiotherapy. After 24 months, 29% of the IMRT patients had grade 2 or worse xerostomia versus 83% in the conventional radiotherapy group. Saliva production was also significantly improved in the IMRT group. The numbers weren't significant enough to establish noninferiority of IMRT, although on the face of it they look promising (18 deaths and 20% local recurrence in the conventional radiotherapy group, compared to 14 deaths but 22% local recurrence after IMRT). The authors estimate a 900-patient trial would be required to confirm a significant difference.
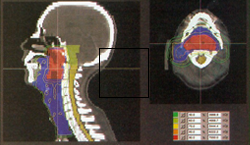
The crucial question is how closely radiation oncologists can delineate the no-treatment zone in IMRT without missing some cancer at the margins, which has been reported with worrisome frequency in the past year. Although IMRT is the hallmark of targeted radiotherapy, in head and neck cancers it faces a moving target. The contours of the malignant region may change from treatment to treatment, due to swallowing, weight loss, edema and shrinkage of the tumor.
Oncologists at MD Anderson are now engaged in a prospective trial of an automated system for adaptive radiation therapy (ART), in which progressive CT images monitor changes in the target area and the treatment contours may be changed daily during the course of IMRT. Real-time monitoring may not be necessary, according to the report in the Journal of Oncology; and it may be more comfortable for the patient if radiation oncologists analyze the data between rather than during treatments. But judging from the feasibility study, say the authors, "we expect ART to evolve briskly towards becoming a commonplace approach for head and neck radiation treatment."