Learning Curve Exists for Esophageal Cancer Surgery
Results of a new Swedish study have shown that a surgeon needed to perform at least 15 esophagectomies in cancer patients in order to achieve stable survival results in the first months after the operation.
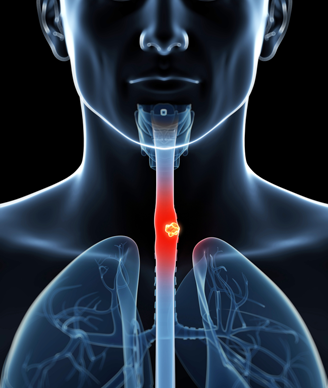
Image © Sebastian Kaulitzki / Shutterstock.com
Results of a new Swedish study have shown that a surgeon needed to perform at least 15 esophagectomies in cancer patients in order to achieve stable survival results in the first months after the operation. In fact, after 15 surgeries the all-cause 30-day mortality decreased by more than half.
However, Jesper Lagergren, a researcher in the department of molecular medicine and surgery at the Karolinska Institutet in Sweden, and colleagues also found that a surgeon has to perform at least 60 operations to achieve optimal long-term survival results.
“What surprised me was that the learning curve for optimizing the long-term prognosis for tumor relapse was so long, and the effect so pronounced,” Lagergren said in a press release. “Our results can guide clinical practice and indicate that a properly organized mentorship and training program should be introduced for esophageal cancer surgery.”
According to the study, no research existed examining the effect of surgical proficiency on long-term mortality in patients undergoing esophagectomy for esophageal cancer. To look at both short- and long-term outcomes, the researchers looked at data from 1,821 patients who had undergone the procedure between 1987 and 2010 with follow-up until 2014. These procedures included 139 surgeons, with a median number of cases performed of 16.
The 30-day mortality for the entire cohort was 5.3%, and the 90-day mortality was 6.4%. Examining first short-term mortality, the data showed that after performing 15 surgeries the 30-day all-cause mortality decreased from 7.9% to 3.1% (P < .001). Ninety-day mortality had a non-significant decrease from 7.3% to 5.2%. When the researchers looked at 30-day mortality from esophageal cancer they found a decrease from 7.3% to 2.5% after 15 cases were performed (P < .001).
“The relatively short length of the proficiency gain curve for short-term mortality parallels published literature from single institutions in open esophagectomy and a national study for minimally invasive esophagectomy in England,” the researchers wrote.
When the researchers looked at 1-year, 3-year, and 5-year mortality they found different change-points associated with significant improvements in mortality. For 1-year mortality, performing at least 53 cases was associated with a reduced mortality from 34.9% to 27.7% (P = .011). For 3-year mortality, performing at least 35 cases was associated with a reduced mortality from 47.4% to 41.5% (P = .49). Finally, for 5-year mortality, performing at least 59 cases was associated with a reduced mortality from 31.4% to 19.1% (P = .006).
“The initial focus of independent surgeon practice is likely to be short-term outcome and, in particular, the 30-day mortality,” the researchers wrote. “When early mortality has been reduced to an acceptable level and when the surgeon gains the technical confidence in performing the procedure, surgeons then can refine their techniques and improve the quality of the resection, which will result in better long-term survival.”