Limited Resection in Duodenal GIST Eliminated Local Recurrence
Limited surgical resection of duodenal gastrointestinal stromal tumors resulted in positive outcomes for both local and systemic disease-free survival, according to the results of a small study.
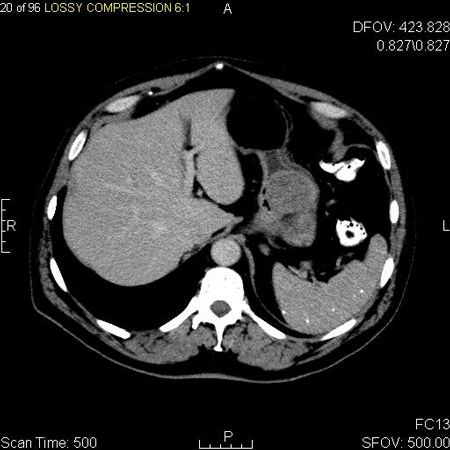
Axial contrast enhanced CT image of a gastrointestinal stromal tumor in the fundus of the stomach; source: Jto410, Wikimedia Commons
Limited surgical resection of duodenal gastrointestinal stromal tumors (GIST) resulted in positive outcomes for both local and systemic disease-free survival, according to the results of a small study recently published in World Journal of Gastrointestinal Surgery.
Because GIST is so heterogeneous, researchers are constantly seeking to define optimal diagnostic approaches and treatments for different subsets of the disease. This study focused on duodenal GIST, which makes up only a small percentage of GIST cases.
For the single-center study, the researchers retrospectively reviewed the records of nine patients who had undergone surgical treatment for duodenal GIST between 2002 and 2011. The median age of patients was 58 years, and patients were followed for a median of 45 months.
Although limited surgical resections are typically simple procedures in patients with gastric GIST, resections in the duodenum are “more challenging,” the researchers wrote.
“The direct proximity to the pancreatic head, the papilla of Vater, and the mesenteric root make limited resections technically demanding and thus, clear resection margins are often barely obtainable,” they wrote.
Sixty-seven percent of patients presented with an initial symptom of gastrointestinal bleeding. A majority of the tumors were found in the first and second part of the duodenum, but were found in all parts among the nine patients.
All patients had undergone limited resection: seven patients had open surgery, one had minimally invasive surgery, and one patient in the group had GIST resection by pancreatoduodenectomy.
When the researchers classified the tumors using Fletcher’s classification scheme, 33% of tumors were considered high risk, 11% were intermediate risk, 44% were low risk, and 11% were very low risk.
No patients developed local recurrence during follow-up, despite the fact that only six of eight patients had microscopically margin-negative resectional status.
“Intraoperatively, all patients of our study showed macroscopically clear resection margins. However, pathohistological examination of the specimens revealed positive margins in two patients after limited resection,” the researchers wrote. “This fact could be a drawback in limited resections of duodenal GIST. Due to the narrow and complex anatomy of the pancreaticoduodenal area with the proximity to the pancreas, the bile duct, the mesenteric root, the portal vein, and the papilla of Vater, clear resection margins of limited resection of duodenal GIST often measure only a few millimeters.”
Seven of the nine patients are alive and considered to be disease-free. One patient died due to tumor progression 3 months post resection; the patient who underwent the pancreatoduodenectomy died of hepatic disease, but had no evidence of local recurrence.