Liver Cancer Screening Improves Survival Rates in Patients With Cirrhosis
A meta-analysis of over 15,000 patients with liver cirrhosis who were diagnosed with hepatocellular carcinoma demonstrates the benefit of screening these patients for liver tumors.
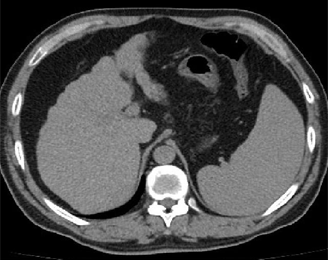
Abdominal CT showing liver cirrhosis; source: Inversitus, Wikimedia Commons.
A new meta-analysis of 15,158 patients with liver cirrhosis who were diagnosed with hepatocellular carcinoma (HCC) demonstrates the benefit of screening this patient population for liver tumors. Patients screened for HCC were more likely to have tumors detected early, to receive curative rather than palliative therapy, and to survive longer. The study was published in Public Library of Science (PLOS) Medicine.
The study authors compiled 47 studies to show that screening with relatively inexpensive blood tests and ultrasound scans could increase liver cancer survival rates in these patients.
Forty-one percent of the patients in this pooled study had their HCC detected through screening, which was associated with a significantly longer survival (odds ratio [OR] = 1.90). Among the patients for whom the data were available, 51% of those who went through HCC screening and 28% of those who did not have survived for at least 3 years after their HCC diagnosis.
HCC surveillance was also associated with improved early-stage detection (OR = 2.08), as well as curative treatment rates (OR = 2.24). Fifty-one percent of patients who were screened received curative therapy compared with 24% of patients who did not undergo screening.
Among those patients who went through screening, the pooled rate of early detection was 71%. Of the patients who did not go through screening and were diagnosed incidentally or who presented with symptoms, only 30% were diagnosed at an early stage of disease.
HCC, when diagnosed at a late stage, is generally untreatable, but if it is diagnosed early, patient outcomes can be improved. Currently, guidelines recommend that patients with hepatitis B be screened about every 6 months, as randomized controlled trials have shown that this type of surveillance can improve outcomes for those hepatitis B patients who are diagnosed with HCC. “These patients should be screened with a simple ultrasound, with or without a serum marker called alpha fetoprotein. Both of these tests are readily available, cheap, and associated with little to no direct risk to patients,” said lead study author Amit Singal, MD, medical director of the Parkland Liver Tumor Clinic at UT Southwestern Medical Center in Dallas.
Similar studies that have examined the benefit of HCC screening have not been conducted in patients with liver cirrhosis, even though patients with cirrhosis have a higher risk of developing liver cancer-annually, about 3% to 5% of patients with cirrhosis develop liver cancer.
“The lack of a randomized trial does not equate to a lack of data supporting efficacy [of screening]. [There is] data that consistently demonstrate that the benefits should provide sufficient rationale to recommend HCC surveillance among patients with cirrhosis,” said Singal.
HCC screening was associated with improved survival, which remained significant in the subset of studies adjusting for lead-time bias, according to the authors.
Still, further studies are needed to confirm these findings, as this current study was a meta-analysis that did not allow for long-term assessment of patient survival and because not all of the studies included adjustment for lead-time bias. Also, none of the studies took into account the potential complications and harms that could be associated with HCC screening, including follow-up liver biopsies after an initial positive cancer diagnosis.
Still, the authors concluded that “these findings provide sufficient evidence to support guidelines that recommend regular HCC surveillance for patients with cirrhosis.”