Long-Term Data Highlights Nilotinib Efficacy, Cardiovascular Effects
Long-term follow-up of a phase II study shows that nilotinib is highly effective in treating chronic phase CML as a first-line therapy, though with relatively common cardiovascular toxicity associated with treatment.
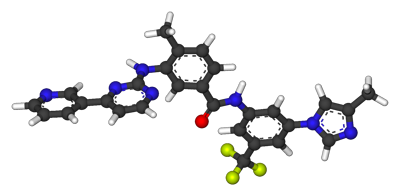
Ball-and-stick model of nilotinib
Long-term follow-up of a phase II study shows that nilotinib is highly effective in treating chronic phase chronic myeloid leukemia (CML) as a first-line therapy, though with relatively common cardiovascular toxicity associated with treatment.
Nilotinib, a second-generation tyrosine kinase inhibitor, was approved as first-line CML therapy based on the ENESTnd trial. The GIMEMA study, reported here, has the longest follow-up yet available on this drug in this setting. It included 73 CML patients enrolled in 2007 and 2008, now with a minimum follow-up of 6 years. Results were published online ahead of print in Haematologica.
Patients in the phase II GIMEMA trial received nilotinib 400 mg twice daily. The median age in the study was 51 years, and 27% were 65 years or older. After 6 years, 75% of the patients remained on the study drug.
The 6-year overall survival (OS) rate was 96%. One patient progressed to blast phase CML while on nilotinib, after 6 months, and died of the disease. Two other patients died while in remission (one with dementia at 75 years old, and one with congestive heart failure at 90 years old). The authors noted that similar to many clinical trials, the median age at diagnosis was lower than in most registries, which could have contributed to the high OS rate.
Thirteen other patients discontinued nilotinib-six of these are now receiving imatinib therapy, three are receiving dasatinib, and four patients are in a trial of treatment-free remission. The primary reason for nilotinib discontinuation was adverse events (11 patients). Most of these (8 patients) were for cardiovascular events, including peripheral arterial obstructive disease, carotid stenosis, angina pectoris, and atrial fibrillation. The median time from initiation of nilotinib therapy to cardiovascular event was 42 months, and the median age at onset was 69 years.
The cumulative probability of achieving major molecular response (MMR) at 6 years was 98%, or 70 of 73 patients. One patient had a confirmed loss of MMR.
“The rate of [cardiovascular adverse events] with the initial dose of 400 mg twice daily remains significant, and supports the use of the lower dose of 300 mg twice daily, as it is currently registered for the front-line treatment of chronic phase CML,” the authors wrote. “The balance between efficacy and safety will depend on the characteristics of the patient and on the goal of therapy, whether it is limited to survival or it is addressed, more ambitiously, to the achievement of a treatment-free remission.”
Targeted Therapy First Strategy Reduces Need for Chemotherapy in Newly Diagnosed LBCL
December 7th 2025Lenalidomide, tafasitamab, rituximab, and acalabrutinib alone may allow 57% of patients with newly diagnosed LBCL to receive less than the standard number of chemotherapy cycles without compromising curative potential.