Low Testosterone May Indicate Prostate Cancer Progression
Low testosterone levels may indicate disease worsening in men diagnosed with low-risk prostate cancer who are being evaluated by active surveillance, according to a new study.
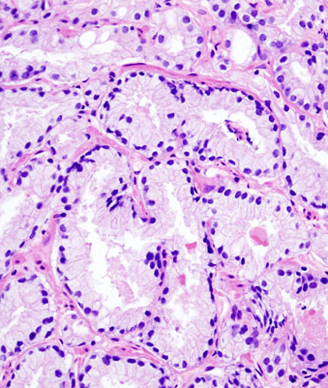
Acinar adenocarcinoma obtained by core needle prostate biopsy; source: KGH, Wikimedia Commons
Low testosterone levels may indicate disease worsening in men diagnosed with low-risk prostate cancer who are being evaluated by active surveillance, according to a new study by Pontificia Universidad Católica de Chile in Santiago, Chile and Beth Israel Deaconess Medical Center in Boston. The results were published in BJU International.
Of a total of 154 men undergoing active surveillance followed for a median of 38 months, 35% (54 men) progressed to active treatment. All of the men were initially diagnosed with low-risk prostate cancer. Those men who transitioned to active treatment had significantly lower free testosterone levels compared with those who continued to have classified low-risk disease (P = .03). The median age of the men was 62, and all were enrolled into the prospective cohort between 2000 and 2012.
Free testosterone levels of less than 0.45 ng/dL had a higher rate of reclassification of initially diagnosed low-risk disease (P = .032) and a several-fold increase in risk of disease reclassification (odds ratio = 4.3). Testosterone levels and a family history of prostate cancer were independent predictors of prostate cancer disease reclassification.
“These results suggest low levels of testosterone are associated with more aggressive prostate cancer. This contradicts long-held beliefs that high testosterone is risky for prostate cancer, and low testosterone is protective,” said lead author Ignacio F. San Francisco, MD, of Pontificia Universidad Católica de Chile, in a statement.
The study found no significant link with total testosterone concentrations in patients. Still, there was a trend of lower overall testosterone levels and increased risk.
Mean age, prostate-specific antigen (PSA), PSA density, body mass index, prostate volume, and testosterone/PSA ratios did not differ between the men whose prostate cancer was reclassified to be higher risk and those who continued with active surveillance.
Free testosterone makes up about 1% to 2% of total testosterone and is considered a surrogate for the portion of circulating testosterone that is biologically active, as this portion of testosterone has been found to correlate more with clinical outcomes compared with total testosterone levels. Much of the rest of circulating testosterone that is not “free” is biologically inactive, bound to sex hormone-binding globulin.
Studies such as this one are attempting to understand changes in biomarkers that may signal higher-risk disease in men undergoing active surveillance, but it is unclear what the factors are that differentiate low-risk vs high-risk early-stage disease. Those men with early-stage but high-risk disease may have a better prognosis with earlier, aggressive prostate cancer treatments.
Further studies with larger cohorts to validate the study results and to identify factors that predict more aggressive early-stage prostate cancer are needed.