Management of Barrett's Esophagus
Barrett's esophagus represents replacement of normal distal esophageal squamous epithelium with specialized columnar epithelium containing goblet cells. Typically arising in the setting of chronic gastroesophageal reflux disease, the presence of Barrett's esophagus carries a 50- to 100-fold increased risk of developing esophageal cancer. Risk factors include male sex, smoking history, obesity, Caucasian ethnicity, age > 50 and > 5-year history of reflux symptoms. Aggressive medical or surgical antireflux therapy may ameliorate symptoms, but have not yet been proven to affect the risk of developing esophageal adenocarcinoma in randomized trials. Although dysplasia is an imperfect biomarker for the development of subsequent malignancy, random sampling of esophageal tissue for dysplasia remains the clinical standard. There have been no studies to establish that endoscopic screening/surveillance programs decrease the rates of death from cancer. Fit patients with Barrett's esophagus and high-grade dysplasia should undergo esophagectomy to prevent the risk of developing esophageal adenocarcinoma. For non–operative candidates, endoscopic ablative approaches may represent a reasonable therapeutic alternative.
Barrett's esophagus represents replacement of normal distal esophageal squamous epithelium with specialized columnar epithelium containing goblet cells. Typically arising in the setting of chronic gastroesophageal reflux disease, the presence of Barrett's esophagus carries a 50- to 100-fold increased risk of developing esophageal cancer. Risk factors include male sex, smoking history, obesity, Caucasian ethnicity, age > 50 and > 5-year history of reflux symptoms. Aggressive medical or surgical antireflux therapy may ameliorate symptoms, but have not yet been proven to affect the risk of developing esophageal adenocarcinoma in randomized trials. Although dysplasia is an imperfect biomarker for the development of subsequent malignancy, random sampling of esophageal tissue for dysplasia remains the clinical standard. There have been no studies to establish that endoscopic screening/surveillance programs decrease the rates of death from cancer. Fit patients with Barrett's esophagus and high-grade dysplasia should undergo esophagectomy to prevent the risk of developing esophageal adenocarcinoma. For non–operative candidates, endoscopic ablative approaches may represent a reasonable therapeutic alternative.
The columnar-lined esophagus was first described in 1906 by the pathologist Tileston, who identified a series of patients with "peptic ulcer of the esophagus."[1] He described a mucus membrane around the ulcer "similar to that found in the stomach." In 1950, Norman Barrett published his treatise on the columnar-lined segment of tissue located within the distal esophagus that now bears his name.[2] Boscher and Taylor were the first to recognize that this specialized epithelium contains the hallmark feature of intestinal-type goblet cells.[3] In 1959, Moersch and associates were the first to suggest that this columnar lining might be a sequela of chronic reflux esophagitis.[4] Over the past 50 years, the association between gastroesophageal reflux, Barrett's esophagus, dysplasia, and adenocarcinoma has been well-established.
Great advances have been made in our understanding and treatment of Barrett's esophagus. Herein we review current concepts in the management of the syndrome.
Clinical Features
Barrett's esophagus is defined as the replacement (metaplasia) of the normal esophageal squamous mucosa with columnar epithelium containing goblet cells. This condition is most commonly diagnosed in the setting of chronic gastroesophageal reflux disease (GERD). Repeated mucosal injury in this setting predisposes patients to the development of mucosal dysplasia and, ultimately, adenocarcinoma. It should therefore be considered a premalignant condition carrying a 50- to 100-fold increased risk of cancer compared with the general population.[5] The risk of developing adenocarcinoma in patients with Barrett's esophagus has been estimated to be 0.5% per year.[6] The incidence of Barrett's esophagus has increased dramatically over the past few decades in conjunction with the associated surge in the frequency of GERD. It remains unproven, however, whether the rising incidence of esophageal adenocarcinoma is caused by an increasing frequency of GERD in the general population.
Risk factors for the development of Barrett's esophagus include male sex, smoking history, obesity, Caucasian ethnicity, age greater than 50 years, and a greater-than-5-year history of reflux symptoms.[7,8] Most patients with Barrett's esophagus have a history of heartburn and acid regurgitation. Less frequent symptoms include dysphagia, chest pain, hematemesis, and melena. Symptoms, however, are unreliable predictors of which patients have Barrett's esophagus, or of who will develop the condition.
Pathophysiology
Barrett's epithelium typically arises in the setting of chronic gastroesophageal reflux. Although acid exposure is believed to play an important role in Barrett's metaplasia, bile reflux may be more closely associated with the development of this condition.[9] Chronic distal esophageal acid inflammation leads to a variety of cellular changes including loss of disaccharidase activity, low mucosal glutaminase levels, and altered levels of mucosal protein synthesis.[8] In addition, a variety of intracellular pathways have been shown to be altered by reflux in the setting of Barrett's metaplasia, including MAP kinase activation[10] and upregulation of COX-2 expression.[11] Bile acids have also been demonstrated to have significant carcinogenic potential. In high concentrations, bile acids have been shown to induce cell membrane and mitochondrial membrane damage, release of reactive oxygen species, and mutation of tumor-suppressor genes such as p53.[12]
Evidence suggests that Barrett's epithelium may progress through a metaplasia-dysplasia-carcinoma sequence. Metaplastic and dysplastic epithelium are frequently found adjacent to each other within pathologic specimens. In addition, progression from metaplasia to low-grade dysplasia, to high-grade dysplasia, and ultimately to adenocarcinoma has been observed in individual patients.[13]
The molecular pathogenesis of Barrett's esophagus and esophageal adenocarcinoma has been shown to include the accumulation of multiple genetic alterations over time. In Barrett's esophagus, loss of heterozygosity of tumor-suppressor genes such as p53, the adenomatous polyposis coli gene (APC), the gene deleted in colorectal cancer (DCC), and MTS1 (p16) has been demonstrated to correlate with progression from metaplasia to dysplasia to cancer.[14] Extensive ongoing work is aimed at determining whether such tumor markers can help clinicians distinguish those patients with Barrett's esophagus who are more likely to progress to adenocarcinoma. Currently available data are insufficient to support the use of these markers during routine clinical practice.
Diagnosis
FIGURE 1
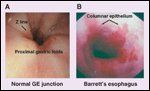
Endoscopic Features of Barrett's Esophagus
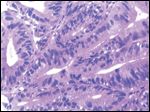
The diagnosis of Barrett's esophagus is achieved at endoscopy (Figure 1), revealing abnormal salmon-colored columnar epithelium extending proximally within the esophagus. The hallmark histologic finding within these specimens is the presence of columnar epithelial metaplasia with mucin-producing goblet cells (Figure 2).
For decades, the diagnosis of Barrett's esophagus was based on the finding of long segments (≥ 3 cm) of columnar epithelium. More recently, intestinal metaplasia has been identified from biopsy specimens of short segments (< 3 cm) of Barrett's esophagus, even in patients with no evidence of GERD.[15] Investigators now recognize that shorter segments of Barrett's esophagus can be associated with the development of adenocarcinoma. Although it would seem logical that the risk of cancer would correlate with the extent of esophageal metaplasia, this notion remains unproven.[16] Currently, patients with long- and short-segment Barrett's esophagus are managed similarly.[17]
Treatment of GERD
FIGURE 2

Histologic Appearance of Barrett's Esophagus
Antireflux therapy is designed to eliminate the signs and symptoms of GERD and to prevent its complications. Both antisecretory therapy (H2 blockers, proton pump inhibitors [PPIs]) and surgical fundoplication have been shown to be effective in reducing or eliminating reflux symptoms (> 90% symptomatic improvement). Despite excellent control of symptoms, no antireflux therapy (medical or surgical) has been definitively proven to promote the regression and/or prevent the progression of Barrett's metaplasia or to decrease the risk of esophageal adenocarcinoma.[17]
Medical Therapy
Antisecretory therapy is directed at acid suppression and is prescribed according to the intensity of GERD symptoms, or based on the severity of the associated esophagitis. Though symptomatic relief can be achieved in the majority of patients, many continue to demonstrate continued acid reflux during pH studies. In fact, up to 80% of patients treated with twice-daily PPIs continue to demonstrate nocturnal gastric acid reflux.[18] Combination regimens employing PPIs and H2 blockers can achieve gastric achlorhydria, leading investigators to speculate whether such medical therapy might have a favorable impact on the natural history of Barrett's esophagus.
A few retrospective studies have been published suggesting that PPIs can promote partial regression of specialized intestinal metaplasia. In a study of 68 patients with acid reflux and proven Barrett's esophagus, profound acid suppression with omeprazole, 40 mg twice daily, was compared with milder acid suppression using ranitidine, 150 mg twice daily. The twice-daily omeprazole regimen reduced reflux symptoms in 99% of patients, and a small but statistically significant regression of Barrett's esophagus was achieved, both in length (6.4%) and in area (7.9%).[19] Malesci and associates similarly demonstrated excellent control of acid exposure with 60 mg of omeprazole every morning, and an associated 53% reduction in length of Barrett's epithelium at endoscopy at 1 year.[20]
Although these studies suggest that aggressive control of acid reflux might be beneficial, such findings do not necessarily translate into a decreased risk of cancer. Therefore, the need for continued surveillance is unchanged. If a patient with no symptoms or esophagitis is found incidentally to have Barrett's esophagus, the decision to prescribe a PPI or other regimen remains controversial.
Emerging data suggest that chronic antisecretory medical therapy might actually enhance the development of cancer. Achlorhydria is a known risk factor for developing adenocarcinoma of the stomach, and is felt to promote the propagation of bacteria that produce carcinogenic nitroso compounds.[21] Acid suppression also increases serum gastrin levels that have been shown to be associated with increased proliferative markers[22] and mucosal hyperplasia[23] in patients with Barrett's esophagus. These findings have yet to be corroborated with clinical trials in humans. In other human studies evaluating the impact of chronic H2-receptor blockade[24] and PPI usage,[25] there was no apparent impact on the risk of developing esophageal adenocarcinoma.
Surgical Therapy
Gastric fundoplication has been postulated to provide a more effective form of antireflux therapy, providing a mechanical barrier to both acid and bile reflux in patients with Barrett's esophagus. Randomized trials to date have not definitively proven this contention, however, with no significant difference reported between medical and surgical antireflux therapy regimens in the prevention of esophageal adenocarcinoma.[26,27] A large case-control study from Sweden[28] and a recent meta-analysis[29] similarly demonstrated no protective effect of antireflux surgery on the development of esophageal adenocarcinoma.
Though not substantiated by prospective, randomized studies to date, several larger nonrandomized series have documented a reduction in the overall risk of cancer progression in patients undergoing fundoplication.[30,31] In a longitudinal analysis of 102 patients with Barrett's esophagus treated medically and/or surgically, 19 patients ultimately developed low-grade dysplasia, 4 developed high-grade dysplasia, and 4 patients progressed to adenocarcinoma with medical treatment alone. None of the patients from this cohort (n = 15) who underwent Nissen fundoplication developed dysplasia or adenocarcinoma.[32]
In a comprehensive review of the outcomes in 97 patients with Barrett's esophagus treated with fundoplication during a median follow-up of 5 years, regression of low-grade dysplasia to a nondysplastic Barrett's epithelium occurred in 44% of patients. No patient developed high-grade dysplasia or cancer in 410 patient-years of follow-up.[33]
In another small randomized study of 59 patients with Barrett's esophagus comparing medical therapy (H2 blockers or omeprazole, n = 27) and surgical therapy (n = 32), a decrease in length of Barrett's esophagus was noted in the surgical arm. Six patients developed dysplasia (five low-grade, one high-grade with early carcinoma) in the medical arm, compared to only one (high-grade with early carcinoma) in the surgical arm. Interestingly, the patient with disease progression in the surgical arm had evidence of failure of the antireflux procedure documented by 24-hour pH analysis. Patients with successful antireflux surgery documented by 24-hour pH studies demonstrated no dysplastic changes or progression to adenocarcinoma.[34]
This principle is further underscored by reports of regression of low-grade dysplasia after successful antireflux procedures, not typically seen with maximal medical therapy regimens. Gurski et al evaluated 91 consecutive patients with Barrett's esophagus receiving either surgical (fundoplication, n = 77) or medical (PPIs, n = 14) therapy.[35] In this series, apparent regression was reported in 28 (36.4%) of 77 patients in the surgical arm vs 1 (7.1%) of 14 in the medical arm. Regression of low-grade dysplasia (17 of 25 patients) to no dysplasia was noted, as well as regression of Barrett's to no Barrett's (11 of 52 patients) in the surgical arm. The median time to regression was 18.5 months. Independent predictors of regression were the presence of a short-segment of Barrett's and antireflux surgery.
In another study, Oelschlager and associates studied the endoscopic outcomes of 106 patients undergoing antireflux surgery in the setting of Barrett's esophagus. Approximately 55% of patients with short-segment Barrett's esophagus were reported to attain complete regression, with only one patient developing cancer in a median 40-month follow-up.[36]
Though such studies are certainly provocative, the concept of regression of Barrett's esophagus remains highly controversial and has not been substantiated by controlled clinical trials. Whether fundoplication ultimately reduces the risk of cancer development also remains unproven. Fundoplication is safe and effective, and can be performed with durable results using minimally invasive techniques. We strongly consider this approach in patients with symptomatic Barrett's esophagus.
High-Grade Dysplasia
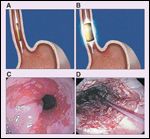
FIGURE 3
High-Grade Dysplasia
High-grade dysplasia is defined histologically as cytologic malignant changes that are confined to the epithelium and do not penetrate the basement membrane (Figure 3). High-grade dysplasia is thought to represent the last step in the neoplastic sequence prior to invasive cancer; it can exist as an isolated lesion or can occur in association with invasive cancer. It should therefore be regarded as both a precursor to, and a marker for, invasive cancer.[37] The natural history of high-grade dysplasia is, in general, not well understood. The cumulative incidence of progression from high-grade dysplasia to esophageal cancer ranges from 16% to 59% in studies spanning 5 to 8 years of follow-up.[38,39]
Detection of high-grade dysplasia is a challenge. Presently, esophagoscopy employing the Seattle protocol (four-quadrant jumbo biopsies taken every 1 cm) remains the best method of detection. Once the diagnosis of high-grade dysplasia is established, confirmation of the diagnosis by an independent pathologist is performed due to the significant interobserver variation in assessing high-grade dysplasia biopsy specimens. Once the diagnosis has been confirmed, several management options exist, including endoscopic surveillance, mucosal ablation, and esophagectomy.
Endoscopic Surveillance
Not all patients with high-grade dysplasia have or will develop cancer.[40] This has led several experts to recommend intensive endoscopic surveillance (every 3–6 months), with invasive therapies being withheld until there is definitive evidence of adenocarcinoma. Since there are no distinctive gross features of high-grade dysplasia at the time of endoscopy, endoscopists rely on random four-quadrant biopsy protocols of the affected segment. Unfortunately, by the time biopsy specimens reveal high-grade dysplasia, 40% to 60% of patients will already have an invasive malignancy.[41]
Extensive work is underway to evaluate methods of enhancing the yield of surveillance protocols utilizing chromendoscopy, high-magnification endoscopy, optical coherence tomography, light-induced fluorescence endoscopy (''LIFE''), and narrow-band imaging.[42] At this time, however, none of these modalities have been clearly established as appropriate for broad use in clinical practice. Existing data fail to clearly demonstrate that current intensive surveillance protocols are cost-effective or that they improve mortality from esophageal cancer.
Endoscopic Ablation
Another option in the treatment of high-grade dysplasia is endoscopic ablation. The goals of endoscopic ablation include destruction of the abnormal Barrett's epithelium, while preserving the overall integrity of the esophagus, minimizing morbidity, and offering a better quality of life. Multiple techniques have been developed to selectively eradicate Barrett's mucosa in an effort to minimize the risk of progression to cancer. Among the most promising modalities are photodynamic therapy (PDT), radiofrequency ablation (RFA), and endoscopic mucosal resection (EMR).
• Photodynamic Therapy-Photodynamic therapy employs a photosensitizing drug that is absorbed and retained at higher concentrations in neoplastic tissue. Light of the proper wavelength (630 nm for porfimer sodium) delivered at the time of endoscopy to the targeted tissues produces an oxidative photochemical reaction that results in mucosal destruction. The endoscopic ablation of Barrett's esophagus with PDT has been evaluated in several studies.
Wang and coworkers from the Mayo Clinic reported their 2-year follow-up of 146 patients with Barrett's esophagus and pathology ranging from no dysplasia to cancer. At the time of last surveillance, nearly one-half the total population of patients had complete ablation of Barrett's esophagus while others had varying degrees of residual metaplasia. Only four patients (2.7%) went on to develop cancer.[43]
Overholt and coworkers have presented the preliminary results of an international, multicenter, randomized, partially blinded trial of PDT and omeprazole (n = 138) vs omeprazole alone (n = 70) in 208 patients with Barrett's esophagus showing high-grade dysplasia.[44] In the PDT/omeprazole group, 77% of patients achieved complete ablation of high-grade dysplasia, compared with 39% in the omeprazole group (P < .0001). In addition, 52% of PDT/omeprazole recipients achieved complete replacement of all Barrett's metaplasia/dysplasia compared with only 7% in the omeprazole group (P < .0001). Although cancer-free survival was substantially improved in the PDT/omeprazole group (P < .0014), 13% of these patients advanced to adenocarcinoma during a mean follow-up of 24.2 months. Strictures occurred in 36% of patients.
The University of Pittsburgh experience includes 50 high-risk patients with either high-grade dysplasia or localized esophageal cancer, with a mean follow-up of 28.1 months. Sixteen patients (32%) are alive with no evidence of disease, 30% are alive with residual or recurrent disease, and 38% have died with recurrent disease. The overall survival at 36 months was 31%. Strictures occurred in 42% of the patients. The intent-to-treat success rate was 38% in cases of high-grade dysplasia and 30% in focal carcinoma.[45]
The primary long-term side effect of PDT, especially with porfimer sodium, is formation of esophageal strictures, which can occur in 20% to 53% of patients. Such strictures are usually responsive to endoscopic dilation. Other complications following PDT include cutaneous photosensitivity, chest pain, nausea, pleural effusions, Candida esophagitis, atrial fibrillation, and odynophagia. Esophageal perforation and tracheo-esophageal fistulas have been reported but are rare (incidence < 1% in most large studies).[46]
The use of steroids has been postulated to reduce stricture formation in the setting of PDT, but Panjehpour and associates found no benefit in the use of oral steroids to prevent the formation of strictures.[47] Another important finding in patients undergoing PDT is the presence of residual patches of subsquamous intestinal metaplasia, occurring in 5% to 50% of cases. Though the biologic significance of residual subsquamous Barrett's remains to be established, concern arises regarding the possibility of ongoing dysplastic progression in these hidden nests of metaplastic tissue.
FIGURE 4
Radiofrequency Ablation of Barrett's Esophagus
• Radiofrequency Ablation-Radiofrequency ablation of Barrett's esophagus is also gaining increased popularity. The ablation system (Halo360 System, BARRX Medical Corporation, Inc, Sunnyvale, Calif) employs balloon-based ablation catheters positioned over a wire. A sizing balloon is initially deployed to measure the inner diameter of the targeted segment. The appropriately sized ablation balloon is then deployed, containing a 3-cm bipolar microelectrode consisting of 60 electrode rings. The electrode rings completely encircle the balloon and alternate in polarity, spaced 250 µm apart. Radiofrequency energy is then delivered to preset levels (10 J/cm2 × 2) at 300 watts in less than 1 second. The catheter can be repositioned to treat the entire length of Barrett's esophagus (Figure 4).
The largest published study to date prospectively evaluated RFA in treating 70 patients with Barrett's esophagus (no dysplasia). At a mean 12-month follow-up, metaplasia was completely eradicated in 70%, and partially eliminated in 25%.[48] Adverse events, including chest discomfort and fever, were rare. The investigators noted no strictures or residual subsquamous metaplasia.
As experience with RFA is acquired, there is an increasing interest in using the procedure, given the promising early results, rare complications, and relative ease of deployment.[49] Prospective, comparative studies will be necessary to elucidate the potential benefit of RFA in the treatment of Barrett's esophagus.
FIGURE 5
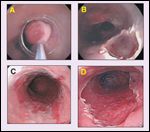
Endoscopic Mucosal Resection
• Endoscopic Mucosal Resection-Endoscopic mucosal resection has also been established as a viable treatment option in patients with nodular or focal high-grade dysplasia. The technique involves raising the mucosal/submucosal target area by intramural saline and/or suction and subsequent snare resection (Figure 5).
The safety of this procedure was evaluated by Seewald and coworkers, who performed EMR on five patients with multifocal high-grade dysplasia or cancer and seven patients with high-grade dysplasia.[50] Complete resections were achieved in all cases, and there were no recurrences in 9 months, although two patients had strictures that were treated with dilation. Giovannini and associates also achieved complete, circumferential resection in 18 of 21 patients with high-grade dysplasia or cancer. All were disease-free after 24 months, except for two local recurrences that were again treated with EMR.[51]
May and coworkers evaluated the results of EMR in the treatment of 115 patients with high-grade dysplasia or early adenocarcinoma. Complete local remission was achieved in 98% of patients, with an associated 3-year survival rate of 88%. Interestingly, a 30% rate of metachronous lesions was observed during the follow-up period, and all but one were treated successfully with repeat EMR.[52] This finding underscores the need for close endoscopic follow-up in patients undergoing local ablative approaches for Barrett's esophagus and associated dysplasia and/or focal intraepithelial carcinoma.
Buttar and associates combined EMR with PDT in treating 17 patients with superficial cancer.[53] Importantly, cancer was seen at the margins of resection in 3 (18%) of the 17 patients. However, 16 (94%) patients achieved and remained in remission at a median follow-up of 13 months. EMR improved staging in 47% of the patients, and esophageal strictures were seen in 30% of the patients after EMR/PDT.
In another large study of 100 consecutive patients evaluating the efficacy of EMR in the treatment of early-stage adenocarcinoma, Ell and coworkers achieved a complete local remission in 99% at an average of 1.9 months. During a mean follow-up of 37.6 months, 11% of patients were found to have recurrent or metachronous carcinomas, all of which were treated successfully with repeat EMR. The estimated 5-year survival rate was 98% in this series.[54]
EMR is now being performed with good success both focally and circumferentially for high-grade dysplasia and early cancer.[55] Complication rates associated with EMR are as high as 30% to 50%, with bleeding being the most common event. Esophageal stricture (especially when EMR is combined with PDT) is a late complication, reported in up to 30% of cases. Perforation risk is less than 1%.
While mucosal ablation techniques are potentially less morbid then esophagectomy, their efficacy remains to be proven in controlled trials. The vast majority of available literature is derived from single-institution, retrospective series. All described ablative techniques have revealed a cohort of patients (2%–60%) that have residual subsquamous Barrett's epithelium. Subsquamous Barrett's epithelium theoretically remains at risk for progression to adenocarcinoma despite continued surveillance endoscopy. At this time, endoscopic ablative therapy for Barrett's esophagus should only be considered appropriate for patients with high-grade dysplasia who are unwilling or unable to undergo esophagectomy.
Esophagectomy
Esophagectomy is the only therapy that can eliminate the risk of progression of dysplasia to cancer.[37] As mentioned above, up to two-thirds of patients with high-grade dysplasia are found to be harboring a cancer in the resected specimen. It is impossible to predict with any certainty who has a malignancy or who will develop one. Fortunately, high-grade dysplasia is highly curable with surgery, with 5-year survival rates exceeding 90%. However, operative mortality rates of 3% to 12% have been reported, and serious postoperative complication rates range from 30% to 50%.
Centers with extensive experience in esophageal resection have minimized the rates of morbidity and mortality, thus maximizing the benefit:risk ratio.[56] Tremendous advances in laparoscopic surgery have made it possible to perform esophagectomy via minimally invasive techniques. Minimally invasive esophagectomy has been developed as a safe and feasible alternative to the traditional open techniques.[57,58] In our recently published experience with 222 minimally invasive esophagectomies, mortality was only 1.4%.[59] Due to the mucosal localization of disease in Barrett's esophagus, minimally invasive esophagectomy for high-grade dysplasia represents an ideal approach for this lesion.[60] This strategy may minimize the morbidity associated with esophageal resection, while providing definitive therapy for even long segments of Barrett's esophagus.[61]
Consensus Recommendations
FIGURE 6

Treatment Algorithm for the Management of Barrett's Esophagus
The Practice Parameters Committee of the American College of Gastroenterology currently recommends that patients with chronic reflux symptoms undergo screening endoscopy for Barrett's esophagus (Figure 6). Barrett's esophagus without evidence of dysplasia can be safely followed with endoscopy at 3-year intervals. The presence of low-grade dysplasia warrants yearly surveillance endoscopy with biopsy. Pathologically confirmed high-grade dysplasia is managed by esophageal resection, mucosal ablation with follow-up surveillance, or intensive endoscopic surveillance (every 3–6 months).[62] Esophagectomy remains the gold-standard treatment for high-grade dysplasia.
As techniques and technology improve, it is likely that ablative strategies will become an important part of the armamentarium in the treatment of Barrett's esophagus. Prospective, controlled studies will be necessary to properly define the optimal role of ablative therapy in this setting.
Financial Disclosure:The authors have no significant financial interest or other relationship with the manufacturers of any products or providers of any service mentioned in this article.
References:
1. Tileston W: Peptic ulcer of the esophagus. Am J Med Sci 132:240-265, 1906.
2. Barrett's NR: Chronic peptic ulcer of the esophagus and "oesophagitis." Br J Surg 38:175-182, 1950.
3. Boscher LH, Taylor FH: Heterotopic gastric mucosa in the esophagus with ulceration and stricture formation. J Thorac Surg 21:306-312, 1951.
4. Moersch RN, Ellis FH, McDonald JR: Pathologic changes occurring in severe reflux esophagitis. Surg Gynecol Obstet 108:476-484, 1959.
5. Cameron AJ, Lomboy CT, Pera M, et al: Adenocarcinoma of the esophagogastric junction and Barrett's esophagus. Gastroenterology 109:1541-1546, 1995.
6. Shaheen NJ, Crosby MA, Bozymski EM, et al: Is there publication bias in reporting cancer risk in Barrett's esophagus? Gastroenterology 119:333-338, 2000.
7. Devesa SS, Blot WJ, Fraumeni JF Jr: Changing patterns in the incidence of esophageal and gastric carcinoma in the United States. Cancer 83:2049-2053, 1998.
8. Peters JH, DeMeester TR: Esophagus: Anatomy, physiology and gastroesophageal reflux disease, in Greenfield LJ, Mulholland MW, Oldham KT, et al (eds): Surgery: Scientific Principles and Practice, 3rd ed, pp 671-675. Philadelphia, Lippincott Williams & Wilkins, 2001.
9. Theisen J, Peters JH, Stein HJ: Experimental evidence for mutagenic potential of duodenogastric juice on Barrett's esophagus. World J Surg 27:1018-1020, 2003.
10. Souza RF, Shewmake K, Pearson S, et al: Acid increases proliferatrion via ERK and p38 MAPK-mediated increases in cyclo-oxygenase-2 in Barrett's adenocarcinoma cells. Am J Physiol Gastrointest Liver Physiol 287:743-748, 2004.
11. Hamoui N, Peters J, Schneider S, et al: Increased acid exposure in patients with gastroesophageal reflux disease influences cyclo-oxygenase-2 gene expression in the squamous epithelium of the lower esophagus. Arch Surg 139:712-717, 2004.
12. Jenkins GJS, D'Souza FR, Suzen SH et al: Deoxycholic acid at neutral and acid pH, is genotoxic to oesophageal cells through the induction of ROS: The potential role of anti-oxidants in Barrett's esophagus. Carcinogenesis 28:136-142, 2007.
13. Hameeteman W, Tytgat GN, Houthoff HJ, et al: Barrett's esophagus: Development of dysplasia and adenocarcinoma. Gastroenterology 96:1249-1256, 1989.
14. Raja S, Finkelstein SD, Bakash FK, et al: Correlation between dysplasia and mutations of six tumor suppressor genes in Barrett's esophagus. Ann Thorac Surg 72:1130-1135, 2001.
15. Spechler SJ, Zeroogian JM, Antonioli DA, et al: Prevalence of metaplasia at the gastro-oesophageal junction. Lancet 344:1533-1536, 1994.
16. Pera M: Trends in incidence and prevalence of specialized intestinal metaplasia, Barrett's esophagus, and adenocarcinoma of the gastroesophageal junction. World J Surg 27: 999-1008, 2003.
17. Castell DO: Medical, surgical and endoscopic treatment of gastoresophageal reflux disease and Barrett's esophagus. J Clin Gastroenterol 33:262-266, 2001.
18. Katz PO, Anderson C, Khouri R, et al: Gastro-oesophageal reflux associated with nocturnal gastric acid breakthrough on proton pump inhibitors. Aliment Pharmacol Ther 1998;12:1231-1234, 1998.
19. Peters FTM, Ganesh S, Kuipers EJ, et al: Endoscopic regression of Barrett's oesophagus during omeprazole treatment; a randomized double-blind study. Gut 45:489-494, 1999.
20. Malesci A, Savarino V, Zentilin P, et al: Partial regression of Barrett's esophagus by long-term therapy with high dose omeprazole. Gastrointest Endosc 44:700-705, 1996.
21. Correa P: Human gastric carcinogenesis: A multi-step and multifactorial process-first American Cancer Society award lecture on cancer epidemiology and prevention. Cancer Res 52:6735,1992.
22. Haigh CR, Attwood SE, Thompson DG, et al: Gastrin induces proliferation in Barrett's metaplasia through activation of the CCK2 receptor. Gastroenterology 124:615-625, 2003.
23. Wetscher GJ, Hinder RA, Smyrk T, et al: Gastric acid blockade with omeprazole promotes gastric carcinogenesis induced by duodenogastric reflux. Dig Dis Sci 44:1132-1135, 1999.
24. Chow WH, Finkle WD, McLaughlin JK, et al: The relation of gastroesophageal reflux disease and its treatment to adenocarcinomas of the esophagus and gastric cardia. JAMA 274:474-477, 1995.
25. Bateman DN, Colin-Jones D, Hartz S, et al: Mortality study of 18,000 patients treated with omeprazole. Gut 52:942-946, 2003.
26. Ye W, Chow WH, Lagergren J, et al: Risk of adenocarcinoma of the esophagus and gastric cardia in patients with gastroesophageal reflux diseases after antireflux surgery. Gastroenterology 121:1286-1293, 2001.
27. Spechler SJ, Lee E, Ahnen D, et al: Long-term outcome of medical and surgical therapies for gastroesophageal reflux disease: Follow-up of a randomized controlled trial. JAMA 285:2331-2338, 2001.
28. Weimin YE, Chow WH, Lagergren J, et al: Risk of adenocarcinomas of the esophagus and gastric cardia in patients with gastroesophageal reflux diseases and after antireflux surgery. Gastroenterology 121:1286-1293, 2001.
29. Corey KE, Schmitz SM, Shaheen NJ: Does a surgical antireflux procedure decrease the incidence of esophageal adenocarcinoma in Barrett's esophagus? A meta-analysis. Am J Gastroenterol 98:2390-2394, 2003.
30. McDonald ML, Trastek VF, Allen MS, et al: Barrett's esophagus: Does an antireflux procedure reduce the need for endoscopic surveillance? J Thorac Cardiovasc Surg 111:1135-1140, 1996.
31. Cameron AJ: Management of Barrett's esophagus. Mayo Clin Proc 73:457-461, 1998.
32. Katz D, Rothstein R, Schned A, et al: The development of dysplasia and adenocarcinoma during endoscopic surveillance of Barrett's esophagus. Am J Gastroenterol 93:536-541, 1998.
33. Hofstetter WL, Peters JH, DeMeester TR, et al: Long-term outcome of antireflux surgery in patients with Barrett's esophagus. Ann Surg 234:532-538, 2001.
34. Ortiz A, DeHaro LFM, Parrilla P, et al: Conservative treatment versus antireflux surgery in Barrett's oesophagus: Long-term results of a prospective study. Br J Surg 83:274-278, 1996.
35. Gurski RR, Peters JH, Hagen JA, et al: Barrett's esophagus can and does regress after antireflux surgery: A study of prevalence and predictive features. J Am Coll Surg 196:706-713, 2003.
36. Oelschlager BK, Barreca M, Chang L, et al: Clinical and pathologic response of Barrett's esophagus to laparoscopic antireflux surgery. Ann Thorac Surg 238: 458 466, 2003.
37. Rice TW, Sontag SJ, Lightdale CJ: Esophagectomy is the treatment of choice for high-grade dysplasia in Barrett's esophagus. Am J Gastroenterol 101: 2177-2184, 2006.
38. Reid BJ, Blount PL, Feng Z, et al: Optimizing endoscopic biopsy detection of early cancers in Barrett's high-grade dysplasia. Am J Gastroenterol 95: 3089-3096, 2000.
39. Buttar NS, Wang KK, Sebo TJ, et al: Extent of high-grade dysplasia in Barrett's esophagus correlates with risk of adenocarcinoma. Gastroenterology 120:1607-1619, 2001.
40. Schnell T, Sontag SJ, Chejfec G, et al: Long-term non-surgical management of Barrett's esophagus with high-grade dysplasia. Gasteroenterology 120:1607-1619, 2001.
41. Dar MS, Goldblum JR, Rice TW, et al: Can extent of high-grade dysplasia in Barrett's esophagus predict the presence of adenocarcinoma at oesophagectomy? Gut 52:486-489, 2003.
42. Schuchert MJ, McGrath K, Buenaventura PO: Barrett's esophagus: Diagnostic approaches and surveillance. Semin Thorac Cardiovasc Surg 17:301-312, 2005.
43. Wang KK: Current status of photodynamic therapy of Barrett's esophagus. Gastrointest Endosc 49:S20-S23, 1999.
44. Overholt BF, Lightdale C, Wang KK, et al: Photodynamic therapy with porfimer sodium for ablation of high grade dysplasia in Barrett's esophagus: International, partially blinded, randomized phase III trial. Gastrointest Endosc 62:488-498, 2005.
45. Schuchert MJ, Luketich JD: Barrett's esophagus-emerging concepts and controversies. J Surg Oncol 95:185-189, 2007.
46. Abbas G, Pennathur A, Keeley SB, et al: Laser ablation therapies for Barrett's esophagus. Semin Thorac Cardiovasc Surg 17:313-319, 2005.
47. Panjehpour M, Overholt BF, Haydek JM, et al: Results of photodynamic for ablation of dysplasia and early cancer in Barrett's esophagus and effect of oral steroids on stricture formation. Am J Gastroenterol 95:2177-2184, 2000.
48. Sharma VK, Wang KK, Overholt BF, et al: Balloon-based, circumferential, endoscopic radiofrequency ablation of Barrett's esophagus: 1-year follow-up of 100 patients. Gastrointest Endosc 65:185-95, 2007.
49. Hazey JW, Dunkin BJ, Melvin WS: Changing attitudes toward endoluminal therapy. Surg Endosc 21:445-448, 2007.
50. Seewald S, Akaraviputh T, Seitz U, et al: Circumferential EMR and complete removal of Barrett's epithelium: A new approach to management of Barrett's esophagus containing high-grade intraepithelial neoplasia and intramucosal carcinoma. Gastrointest Endosc 57:854-859, 2003.
51. Giovannini M, Bories E, Pesenti C, et al: Circumferential endoscopic mucosal resection in Barrett's esophagus with high grade intraepithelial neoplasia or mucosal cancer: Preliminary results in 21 patients. Endoscopy 36:782-787, 2004.
52. May A, Gossner L, Pech O, et al: Local endoscopic therapy for intra-epithelial high-grade neoplasia and early adenocarcinoma in Barrett's oesophagus: Acute-phase and intermediate results of a new treatment approach. Eur J Gastroenterol Hepatol 14:1085-1091, 2002.
53. Buttar NS, Wang KK, Lutzke LS, et al: Combined endoscopic mucosal resection and photodynamic therapy for esophageal neoplasia within Barrett's esophagus. Gastroinest Endosc 54:682-688, 2001.
54. Ell C, May A, Pech O, et al: Curative endoscopic resection of early esophageal adenocarcinomas (Barrett's cancer). Gastrointest Endosc 65:3-10, 2007.
55. Lopes CV, Hela M, Pesenti C, et al: Circumferential endoscopic resection of Barrett's esophagus with high-grade dysplasia or early adenocarcinoma. Surg Endosc 21:820-824, 2007.
56. Swisher SG, Deford L, Merriman KW, et al: Effects of operative volume on morbidity, mortality and hospital use after esophagectomy for cancer. J Thorac Cardiovasc Surg 119:1126-1132, 2000.
57. Luketich JD, Nguyen NT, Schauer P: Laparoscopic transhiatal esophagectomy for Barrett's esophagus with high-grade dysplasia. J Soc Lap Surg 2:75-77, 1998.
58. Pierre AF, Luketich JD. Technique and role of minimally invasive esophagectomy for premalignant and malignant diseases of the esophagus. Surg Oncol Clin N Am 11:337-350, 2002.
59. Luketich JD, Alvelo-Rivera M, Buenaventura PO, et al: Minimally-invasive esophagectomy: Outcomes in 222 patients. Ann Surg 238:486-494, 2003.
60. Nguyen NT, Schauer P, Luketich JD: Minimally invasive esophagectomy for Barrett's esophagus with high-grade dysplasia. Surgery 127:284-290, 2000.
61. Pennathur A, Landreneau RJ, Luketich JD: Surgical aspects of the patient with high-grade dysplasia. Semin Thorac Cardiovasc Surg 17:326-332, 2005.
62. Sampliner RE: Updated guidelines for the diagnosis, surveillance and therapy of Barrett's esophagus. Am J Gastroenterol 97:1888-1895, 2002.