Triple-negative breast cancer, which affects about 10% of older women with breast cancer, represents a major treatment challenge in this population. Treatment decisions for these patients can best be made based on geriatric assessment, estimated life expectancy, whether the treatment goal is prolonged survival or palliation, the potential benefits and toxicities of a specific treatment, and the patient’s personal goals for treatment. Treatment outcomes for healthy older and younger women are similar, but great challenges exist in managing the vulnerable and frail patient. The cornerstone of therapy for early-stage triple-negative breast cancer is local therapy (surgery and radiation) and, for most patients, adjuvant chemotherapy. In the management of metastatic triple-negative breast cancer, all therapy is palliative and chemotherapy is the treatment of choice. Since all treatment modalities in older patients-especially chemotherapy-can affect physical and mental function, a geriatric assessment is key in selecting the most appropriate treatment strategy. Many older patients (older than 70 years) are poor candidates for state-of-the-art therapy, and some who have substantial comorbidities not related to breast cancer may opt for palliative and hospice care. In this review, we will discuss the role of geriatric assessment, alternative treatment modalities for older women with triple-negative breast cancer, and other special considerations for this patient population.
Introduction
Breast cancer is the leading cancer diagnosis among women in the United States, accounting for approximately one in three cancers, and it is the second leading cause of cancer-related death in women.[1] Based on data from the Surveillance, Epidemiology, and End Results (SEER) Program of the National Cancer Institute, the median age at breast cancer diagnosis for women in the United States is 62 years, and among patients with breast cancer the average age at death is 68 years.[2] Since the second half of the 20th century, major improvements in public health and advances in medical care have led to significant increases in life expectancy in the United States, with the female population aged 65 years and older expected to grow from 26.4 million in 2015 to an estimated 46.2 million in 2050.[3] This 80% increase will result in an absolute increase in the number of older women with breast cancer.
Triple-negative breast cancer represents a distinct phenotype of breast cancer characterized by rapid tumor growth, a relapse rate that peaks in the first 2 to 3 years after diagnosis, and an increased incidence in African-American and Hispanic populations. While increasing age is generally associated with a decreasing incidence of triple-negative breast cancer, in one SEER study (N = 57,483), triple-negative breast cancer was diagnosed in approximately 10% of breast cancer patients over 65 years of age.[4] In another registry-based study of 771 patients with stages I to III triple-negative breast cancer, 159 (21%) were 65 years of age and older.[5] Notably, in the latter study, patients older than 65 were significantly less likely to receive chemotherapy (61% of patients over 75 years of age did not receive chemotherapy, compared with 5% of patients younger than 64 years; P < .001), and 12% of patients in this older age group were not evaluated by an oncologist. Regardless of cancer type, the management of older patients with cancer is characterized by less treatment compared with younger patients; in breast cancer, this conservative approach has been shown to result in poorer breast cancer–specific survival in older patients compared with younger ones.[6]
Genetic subtyping has shown that triple-negative breast cancer is associated with the basal-like subtype, which occurs less frequently in older patients. In a cohort of 3,947 patients with triple-negative breast cancer, molecular subtyping as determined by the PAM50 breast cancer gene expression assay showed that the basal-like subtype was found in 44% of patients aged 21 to 39 years, in 22% of patients aged 50 to 59 years, and in 9% of patients aged 70 to 93 years.[7] In the group with triple-negative breast cancer, after controlling for subtype, treatment, tumor size, nodal status, and grade, age had no impact on either disease-free or overall survival.
The treatment of triple-negative breast cancer is challenging, given that chemotherapy is the only available systemic therapy for these patients. Since chemotherapy can be associated with severe toxicity, management challenges with this breast cancer subtype are even greater in older patients, who may also have a greater incidence of comorbid illness, use of multiple medications, and preexisting functional loss, such that treatment-related toxicity may dramatically alter their daily function and quality of life. In this review, we provide recommendations for the care of older patients with triple-negative breast cancer, including assessment of functional status, estimation of toxicity risk and survival, and management approaches to consider for older patients with early or metastatic disease.
Geriatric Assessment
A key characteristic of the aging process is a cumulative decline in the function of multiple physiologic systems. This results in decreased organ function reserve, as well as comorbidity, frailty, and limited ability to tolerate stressors such as infections or chemotherapy.[8] These declines and resultant physiologic deficits occur at varying rates in different individuals and organ systems, so that there may be vast differences in life expectancy, functional status, and health status among patients of identical chronologic ages. Geriatric assessment is a multidimensional interdisciplinary evaluation that can be used to identify patient-related health problems by summarizing key features of an older adult’s physical function as well as information about polypharmacy, comorbidities, nutritional status, cognitive status, and psychosocial status. Many deficits uncovered by geriatric assessment are not detected on routine clinical evaluation. In one large study, one or more geriatric assessment–identified deficits were found in 69% of patients with a normal Karnofsky Performance Status score.[9] The identified deficits included polypharmacy, impairments in cognitive function, and impairments in instrumental activities of daily living. In another study, only 10% of older cancer patients with geriatric assessment–identified falls had appropriate clinician documentation in their medical records, and even fewer (6%) had referrals for evidence-based interventions for fall prevention.[10] Identifying these deficits is particularly important because they are independent predictors of poor survival outcomes that could potentially attenuate the benefit of chemotherapy in older women with triple-negative breast cancer.[11]
Life Expectancy
Regardless of their particular diagnosis, most breast cancer patients who develop recurrence do so within 2 to 3 years after the initial diagnosis. Accurate estimation of life expectancy is essential in selecting treatment for older adults with cancer, especially for frail patients for whom the potential survival benefit of adjuvant chemotherapy may be nullified by competing medical comorbidities. Several validated online tools are available that enable accurate estimates to be made, and which may incorporate geriatric assessment variables in addition to demographic and clinical data (eg, https://eprognosis.ucsf.edu/calculators).[12]
Chemotherapy Toxicity
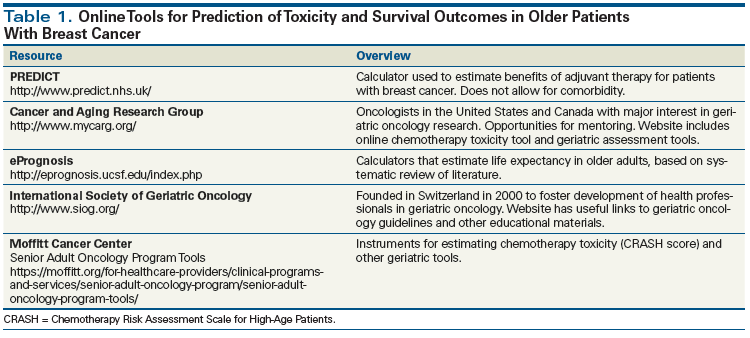
Not only is the geriatric assessment a valuable instrument for predicting the potential benefits of chemotherapy, but it can also be used to assess the potential toxicities of chemotherapy. In a pivotal study of 500 patients, geriatric assessment–identified deficits-including falls and hearing impairment, but not Karnofsky Performance Status scores-were shown to predict the risk of grades 3 and 4 chemotherapy toxicity.[13,14] This validated model and others[15] are available online (Table 1). The geriatric assessment can also identify deficits for which targeted evidence-informed interventions are available that can improve outcomes. In a classic study, cancer patients randomized postoperatively to three home visits and five telephone contacts by an advanced practice nurse survived significantly longer than patients randomized to usual care (mortality rates in the whole cohort, 22% vs 28%). The major benefit was among those with more advanced cancer stage (2-year survival, 67% vs 40% favoring the intervention group).[16] Since then, other studies have shown that geriatric assessment interventions can lead to improvement in quality of life and may help with chemotherapy decision making.[17-19]
Four Key Steps in Making Treatment Decisions for Older Patients With Triple-Negative Breast Cancer
Following initial screening and preferably a geriatric assessment, management of the older patient with triple-negative breast cancer can be broken down into four steps:
• First, determine whether the medical goal of treatment is to improve the chance for cure (the goal of treatment in the adjuvant setting) or palliation, and convey this information to the patient and family.
• Second, query the patient as to what is important to her and what her goals are for being treated. The patient and family may not always agree on these goals, and it is critical that discord be resolved early.
• Third, using geriatric assessment–based data and appropriate tools and models, including estimates of life expectancy for the individual patient, calculate the risks and benefits of treatment.
• Last, present these risks-and-benefits data to the patient and family using shared decision making and in language that they can understand, to finalize the plan for care.
Management of Early-Stage Triple-Negative Breast Cancer
Local/regional therapy
For the majority of older women with triple-negative breast cancer, core biopsy will establish a definitive diagnosis, and for most of these patients management should be similar to that of younger women. Breast conservation should be offered when appropriate, with the goal of no ink on the tumor margin.[20] Sentinel node sampling has replaced axillary dissection for a clinically negative axilla and in patients with one to two positive sentinel nodes and a clinically negative axilla[21]; further axillary dissection is unnecessary for patients who will receive locoregional irradiation.[22] For patients with positive sentinel nodes, axillary radiotherapy represents an appropriate alternative to axillary lymph node dissection.[21,23] Recently there has been interest in the use of accelerated partial breast irradiation as an alternative to whole-breast radiotherapy, but the suitability of the former approach in women with triple-negative breast cancer is uncertain.[24,25]
Management of Older Patients With Unresectable Triple-Negative Breast Cancer
Older patients with triple-negative breast cancer whose tumors are too large for surgical resection or who are too frail for neoadjuvant chemotherapy represent a major clinical challenge. Those who can tolerate neoadjuvant therapy can be treated with anthracycline and taxane regimens (which will be discussed later in this article). In the neoadjuvant setting, the addition of carboplatin to anthracyclines and taxanes significantly improves the pathologic complete response rate, but whether overall survival is also improved is uncertain.[26]Nonanthracycline regimens may also be extremely effective, and represent a good option for those with borderline or poor cardiac function; in one large series (N = 190), a docetaxel and carbopla tin combination administered for 6 cycles was associated with an average pathologic complete response rate of 55%.[27] The role of platinums for neoadjuvant and adjuvant treatment of triple-negative breast cancer remains controversial for patients of all ages and is under active investigation. Older fit patients who are being considered as candidates for adjuvant therapy should be offered participation in clinical trials evaluating the role of platinums in the adjuvant setting. An example of such a trial is the NRG Oncology trial BR003 (ClinicalTrials.gov identifier: NCT02488967), which is testing adjuvant weekly paclitaxel with or without carboplatin (following a regimen of anthracycline-based chemotherapy) in patients with node-positive or high-risk triple-negative breast cancer. For patients unfit for systemic chemotherapy, radiotherapy alone (primary irradiation) may be used. In one large series of more than 450 breast cancer patients treated with radiation alone at doses of 70 to 80 Gy, the 3-year local control rates were 81%, 71%, 61%, and 36% for tumors less than 4 cm, 4 to 6 cm, 6 to 8 cm, and greater than 8 cm, respectively. In general, doses higher than 60 Gy are needed to achieve durable local control in the absence of surgical excision.[28] In another series of patients treated with radiation alone, the 10-year local control rate was 70% for patients with T3 tumors (but hormone receptor status was not available).
Systemic therapy
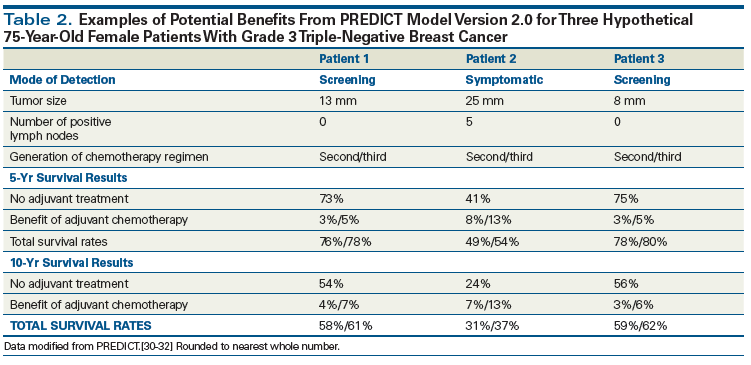
In patients with triple-negative breast cancer, the majority of relapses occur less than 5 years from diagnosis,[29] and chemotherapy is not likely to be of value to patients with short life expectancy. We suggest calculating the benefits of chemotherapy using the PREDICT model (http://www.predict.nhs.uk/predict_v2.0.html),[30] which provides 5- and 10-year survival estimates of the benefits of chemotherapy based on patient age and clinical factors (although this model is less accurate in older women and in women with hormone receptor–negative tumors).[31,32] Another drawback of the model in older patients is that only information on all-cause mortality is provided, making it difficult to separate death due to breast cancer from death not related to breast cancer. In spite of these shortfalls, the PREDICT model provides a reasonable estimate of overall survival at 5 and 10 years, and likely is better at estimating the potential benefits of treatment than an “educated guess” would be. Much as with other recommended guidelines, we suggest that chemotherapy be discussed with women who have a projected overall survival benefit of 3% to 5% at 10 years, and that chemotherapy be considered when its 10-year survival benefit exceeds 5%.[33]
Fit older women with triple-negative breast cancer benefit from standard adjuvant chemotherapy. In one large trial, standard chemotherapy with 4 cycles of doxorubicin and cyclophosphamide or 6 cycles of an oral-based cyclophosphamide, methotrexate, and fluorouracil regimen was superior to treatment with oral capecitabine.[29] Second-generation regimens (eg, docetaxel and cyclophosphamide [TC]) and third-generation regimens that include both anthracyclines and taxanes yield better survival outcomes than first-generation regimens and are preferred in most fit older patients. We suggest using a nonanthracycline regimen such as 4 to 6 cycles of TC rather than an anthracycline and taxane regimen, unless the latter regimen improves the patient’s estimated 5-year survival by more than 2% in the PREDICT model. We believe that a difference of more than 2% is enough to account for the limitations of the model in older women and those with hormone receptor–negative tumors. This represents a tradeoff for less toxicity vs questionably shorter survival for the nonanthracycline regimen. Table 2 shows estimates of the benefit of therapy and the major difference in potential benefits for third-generation vs second-generation regimens for three hypothetical patients with average comorbidity using the PREDICT model.[34,35]
KEY POINTS
- Geriatric assessment is a multidimensional interdisciplinary evaluation that frequently discovers deficits that are not detected during routine clinical evaluation.
- Life expectancy evaluation is important for decision making and can be easily calculated using online tools.
- Older patients with triple-negative breast cancer derive similar benefits from adjuvant chemotherapy compared with younger patients, but are at greater risk for toxicity.
- Metastatic triple-negative breast cancer in older patients is usually best treated with single-agent sequential therapy, and treatment choice should be based on the toxicity profile of the agent.
There are major toxicity considerations for patients receiving chemotherapy. The TC regimen has been tested in older fit patients and appears to be reasonably well tolerated.[36] Administration of granulocyte growth factors is necessary with the use of this regimen. Anthracyclines and taxanes are associated with major short-term toxicity in older patients and require close monitoring. Long-term risks include acute myeloid leukemia and congestive heart failure.[37,38] Cardiac function should be measured prior to administration of the anthracycline. Another major concern is the development of taxane-related neuropathy, which even when mild can be a clinically significant issue in older patients. Patients should be assessed before each dose of taxane for both motor and sensory loss. Using models that predict high-grade toxicities (grade 3 and higher) can help identify which older patients are most likely to experience side effects and guide treatment selection.[13,15] The potential risk for hospitalization secondary to chemotherapy should also be considered. In one study, among patients 65 years of age and older, hospitalization for toxicity occurred in 13% of patients treated with TC; in 24% of patients treated with the regimen of docetaxel, doxorubicin, and cyclophosphamide; and in about 20% of patients who received anthracycline/taxane regimens.[39] Since hospitalization can cause functional decline and shortened survival times,[40] these risks should be considered in treatment selection.
Metastatic disease
Metastatic breast cancer remains incurable regardless of patient age, and all treatment is palliative. The median survival time for patients with metastatic triple-negative breast cancer is approximately 14 months[41]; in general, older age is a risk factor for early death (within 1 month of diagnosis) in those who present with de novo metastatic breast cancer.[42] The goals of therapy in patients with metastases are to maintain the highest function and quality of life for as long as possible.[43] For older patients with symptomatic brain and bone metastases, radiotherapy should be considered. The general approach to treating older patients with metastatic triple-negative breast cancer is similar to that followed in younger patients; it consists of using single agents sequentially, except for patients with rapidly progressive symptomatic metastases.
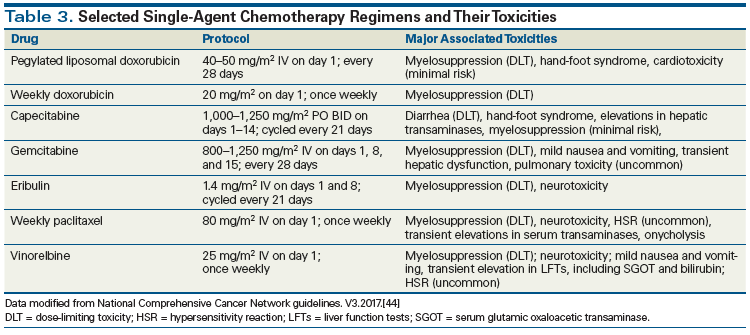
Several single agents recommended as preferred single agents by the National Comprehensive Cancer Network have been studied in older patients (Table 3).[44] Capecitabine, weekly paclitaxel, nab-paclitaxel, eribulin (as second- and third-line treatment), liposomal doxorubicin, vinorelbine, and gemcitabine have been studied in older populations, and the choice should be based on toxicity profile. As first-line treatment, response rates vary greatly according to patient characteristics and average about 30% to 50%, while progression-free survival averages about 3 to 6 months. Second- and third-line therapies are less effective. Several new agents show promise. Olaparib, a poly (ADP-ribose) polymerase inhibitor, was associated with a significant improvement in progression-free survival when compared with the treating physician’s choice of therapy (7 months vs 4.2 months) in a phase III trial of patients with BRCA germline mutations; however, as with most trials of newer agents, only a small number of patients (n = 15) were 65 years of age and older.[45] Modulating the immune system using checkpoint inhibitors also shows promise, but almost no data are available in older breast cancer patients.[46] While frail older patients may occasionally benefit from chemotherapy, for most the value of chemotherapy will be modest at best; these patients should all be considered for palliative and hospice care.
Conclusions
The number of older patients with triple-negative breast cancer will continue to grow as the population ages. Unfortunately, there is a paucity of clinical trial data pertaining to treatment of cancer in the elderly, and many practice-changing breast cancer trials over the last decade have included only a small percentage of older patients.[47-49] Although it is unlikely that this shortcoming will be mitigated quickly, major efforts are underway to expand the information pool regarding risks and benefits of cancer treatment in older patients.[47] Perhaps “big data” will help provide genetic and genomic information that will help us to evaluate the safety of the many new treatment modalities in the community setting; however, even if this is the case, key information-such as the effects of treatment on physical and cognitive function-is likely to be lacking. Clinicians should offer clinical trial participation to all fit older women with triple-negative breast cancer who meet the eligibility criteria. Trials focused on less fit and frail older patients with triple-negative breast cancer are also sorely needed.
Financial Disclosure:The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. DeSantis C, Ma J, Bryan L, Jemal A. Breast cancer statistics, 2013. CA Cancer J Clin. 2014;64:52-62.
2. National Cancer Institute Surveillance, Epidemiology, and End Results Program. Cancer stat facts: female breast cancer. http://seer.cancer.gov/statfacts/html/breast.html. Accessed January 6, 2018.
3. United Nations Department of Economic and Social Affairs, Population Division. World population ageing 2015. http://www.un.org/en/development/desa/population/theme/ageing/WPA2015.shtml. Accessed January 6, 2018.
4. Howlader N, Altekruse SF, Li CI, et al. US incidence of breast cancer subtypes defined by joint hormone receptor and HER2 status. J Natl Cancer Inst. 2014;106:dju055.
5. Kaplan HG, Malmgren JA, Atwood MK. Triple-negative breast cancer in the elderly: prognosis and treatment. Breast J. 2017;23:630-7.
6. Smith BD, Jiang J, McLaughlin SS, et al. Improvement in breast cancer outcomes over time: are older women missing out? J Clin Oncol. 2011;29:4647-53.
7. Jenkins EO, Deal AM, Anders CK, et al. Age-specific changes in intrinsic breast cancer subtypes: a focus on older women. Oncologist. 2014;19:1076-83.
8. Sawhney R, Sehl M, Naeim A. Physiologic aspects of aging: impact on cancer management and decision making, part I. Cancer J. 2005;11:449-60.
9. Jolly TA, Deal AM, Nyrop KA, et al. Geriatric assessment-identified deficits in older cancer patients with normal performance status. Oncologist. 2015;20:379-85.
10. Guerard EJ, Deal AM, Williams GR, et al. Falls in older adults with cancer: evaluation by oncology providers. J Oncol Pract. 2015;11:470-4.
11. Robb C, Boulware D, Overcash J, Extermann M. Patterns of care and survival in cancer patients with cognitive impairment. Crit Rev Oncol Hematol. 2010;74:218-24.
12. Yourman LC, Lee SJ, Schonberg MA, et al. Prognostic indices for older adults: a systematic review. JAMA. 2012;307:182-92.
13. Hurria A, Togawa K, Mohile SG, et al. Predicting chemotherapy toxicity in older adults with cancer: a prospective multicenter study. J Clin Oncol. 2011;29:3457-65.
14. Hurria A, Mohile S, Gajra A, et al. Validation of a prediction tool for chemotherapy toxicity in older adults with cancer. J Clin Oncol. 2016;34:2366-71.
15. Extermann M, Boler I, Reich RR, et al. Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer. 2012;118:3377-86.
16. McCorkle R, Strumpf NE, Nuamah IF, et al. A specialized home care intervention improves survival among older post-surgical cancer patients. J Am Geriatr Soc. 2000;48:1707-13.
17. Caillet P, Canoui-Poitrine F, Vouriot J, et al. Comprehensive geriatric assessment in the decision-making process in elderly patients with cancer: ELCAPA study. J Clin Oncol. 2011;29:3636-42.
18. Lapid MI, Rummans TA, Brown PD, et al. Improving the quality of life of geriatric cancer patients with a structured multidisciplinary intervention: a randomized controlled trial. Palliat Support Care. 2007;5:107-14.
19. Kenis C, Bron D, Libert Y, et al. Relevance of a systematic geriatric screening and assessment in older patients with cancer: results of a prospective multicentric study. Ann Oncol. 2013;24:1306-12.
20. Moran MS, Schnitt SJ, Giuliano AE, et al. Society of Surgical Oncology–American Society for Radiation Oncology consensus guideline on margins for breast-conserving surgery with whole-breast irradiation in stages I and II invasive breast cancer. Int J Radiat Oncol Biol Phys. 2014;88:553-64.
21. Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305:569-75.
22. Donker M, van Tienhoven G, Straver ME, et al. Radiotherapy or surgery of the axilla after a positive sentinel node in breast cancer (EORTC 10981-22023 AMAROS): a randomised, multicentre, open-label, phase 3 non-inferiority trial. Lancet Oncol. 2014;15:1303-10.
23. Galimberti V, Cole BF, Zurrida S, et al. Axillary dissection versus no axillary dissection in patients with sentinel-node micrometastases (IBCSG 23-01): a phase 3 randomised controlled trial. Lancet Oncol. 2013;14:297-305.
24. Smith BD, Arthur DW, Buchholz TA, et al. Accelerated partial breast irradiation consensus statement from the American Society for Radiation Oncology (ASTRO). Int J Radiat Oncol Biol Phys. 2009;74:987-1001.
25. Fyles AW, McCready DR, Manchul LA, et al. Tamoxifen with or without breast irradiation in women 50 years of age or older with early breast cancer. N Engl J Med. 2004;351:963-70.
26. Sikov WM, Berry DA, Perou CM, et al. Impact of the addition of carboplatin and/or bevacizumab to neoadjuvant once-per-week paclitaxel followed by dose-dense doxorubicin and cyclophosphamide on pathologic complete response rates in stage II to III triple-negative breast cancer: CALGB 40603 (Alliance). J Clin Oncol. 2015;33:13-21.
27. Sharma P, Lopez-Tarruella S, Garcia-Saenz JA, et al. Efficacy of neoadjuvant carboplatin plus docetaxel in triple-negative breast cancer: combined analysis of two cohorts. Clin Cancer Res. 2017;23:649-57.
28. Arriagada R, Mouriesse H, Sarrazin D, et al. Radiotherapy alone in breast cancer. I. Analysis of tumor parameters, tumor dose and local control: the experience of the Gustave-Roussy Institute and the Princess Margaret Hospital. Int J Radiat Oncol Biol Phys. 1985;11:1751-7.
29. Muss HB, Berry DA, Cirrincione CT, et al. Adjuvant chemotherapy in older women with early-stage breast cancer. N Engl J Med. 2009;360:2055-65.
30. Wishart GC, Bajdik CD, Dicks E, et al. PREDICT Plus: development and validation of a prognostic model for early breast cancer that includes HER2. Br J Cancer. 2012;107:800-7.
31. Englehardt EG, Garvelink MM, de Haes JH, et al. Predicting and communicating the risk of recurrence and death in women with early-stage breast cancer: a systematic review of risk prediction models. J Clin Oncol. 2014;32:238-50.
32. van Maaren MC, van Steenbeek CD, Pharoah PDP, et al. Validation of the online prediction tool PREDICT v. 2.0 in the Dutch breast cancer population. Eur J Cancer. 2017.;86:
364-72.
33. Wishart GC, Bajdik CD, Azzato EM, et al. A population-based validation of the prognostic model PREDICT for early breast cancer. Eur J Surg Oncol. 2011;37:411-7.
34. Wishart GC, Azzato EM, Greenberg DC, et al. PREDICT: a new UK prognostic model that predicts survival following surgery for invasive breast cancer. Breast Cancer Res. 2010;12:R1.
35. National Health Service, United Kingdom. PREDICT tool version 2.0: breast cancer overall survival; input. http://www.predict.nhs.uk/predict_v2.0.html. Accessed January 8, 2018.
36. Freyer G, Campone M, Peron J, et al. Adjuvant docetaxel/cyclophosphamide in breast cancer patients over the age of 70: results of an observational study. Crit Rev Oncol Hematol. 2011;80:466-73.
37. Freedman RA, Seisler DK, Foster JC, et al. Risk of acute myeloid leukemia and myelodysplastic syndrome among older women receiving anthracycline-based adjuvant chemotherapy for breast cancer on Modern Cooperative Group Trials (Alliance A151511). Breast Cancer Res Treat. 2017;161:363-73.
38. Muss HB, Berry DA, Cirrincione C, et al. Toxicity of older and younger patients treated with adjuvant chemotherapy for node-positive breast cancer: the Cancer and Leukemia Group B experience. J Clin Oncol. 2007;25:3699-704.
39. Barcenas CH, Niu J, Zhang N, et al. Risk of hospitalization according to chemotherapy regimen in early-stage breast cancer. J Clin Oncol. 2014;32:2010-7.
40. Drubbel I, Numans ME, Kranenburg G, et al. Screening for frailty in primary care: a systematic review of the psychometric properties of the frailty index in community-dwelling older people. BMC Geriatr. 2014;14:27.
41. Kassam F, Enright K, Dent R, et al. Survival outcomes for patients with metastatic triple-negative breast cancer: implications for clinical practice and trial design. Clin Breast Cancer. 2009;9:29-33.
42. Vaz-Luis I, Lin NU, Keating NL, et al. Factors associated with early mortality among patients with de novo metastatic breast cancer: a population-based study. Oncologist. 2017;22:386-93.
43. Jolly T, Williams GR, Jones E, Muss HB. Treatment of metastatic breast cancer in women aged 65 years and older. Womens Health (Lond). 2012;8:455-71.
44. National Comprehensive Cancer Network. Dosing schedules for chemotherapy regimens for recurrent or metastatic breast cancer. In: NCCN clinical practice guidelines in oncology: breast cancer. Version 3.2017. November 10, 2017. https://www.nccn.org/professionals/physician_gls/pdf/breast.pdf. Accessed January 6, 2018.
45. Robson M, Im SA, Senkus E, et al. Olaparib for metastatic breast cancer in patients with a germline BRCA mutation. N Engl J Med. 2017;377:523-33.
46. Adams S, Schmid P, Rugo HS, et al. Phase 2 study of pembrolizumab (pembro) monotherapy for previously treated metastatic triple-negative breast cancer (mTNBC): KEYNOTE-086 cohort A. J Clin Oncol. 2017;35(suppl):abstr 1008.
47. Hurria A, Levit LA, Dale W, et al. Improving the evidence base for treating older adults with cancer: American Society of Clinical Oncology statement. J Clin Oncol. 2015;33: 3826-33.
48. Strulov Shachar S, Hurria A, Muss HB. Targeted therapies in older adults with breast cancer: what do we know? J Clin Oncol. 2016;34:3486-8.
49. Freedman RA, Foster JC, Seisler DK, et al. Accrual of older patients with breast cancer to Alliance systemic therapy trials over time: protocol A151527. J Clin Oncol. 2017;35:421-31.