MRI Could Aid Breast Cancer Detection in Average-Risk Women
A new study found that magnetic resonance imaging (MRI) screening improved the detection of small, high-grade breast cancers in women with average risk.
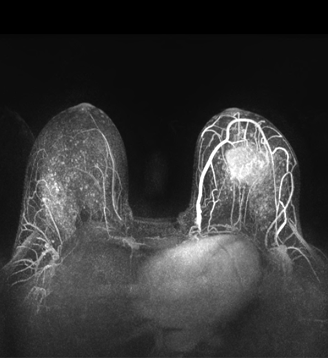
MRI showing invasive breast cancer
A new study found that magnetic resonance imaging (MRI) screening improved the detection of small, high-grade breast cancers in women with average risk. The study, presented at the 2015 American Society of Clinical Oncology (ASCO) Breast Cancer Symposium in San Francisco, suggested that MRI screening every 3 years may be sufficient to establish an interval cancer rate of zero (abstract 1).
“Mammography consistently fails to detect rapidly growing cancers, which will then be detected as ‘interval cancers,’” said Christiane Kuhl, MD, of the University of Aachen in Germany, who presented the study. “MRI has so far been used only in high-risk women, there is no evidence of its use in average-risk women.”
In the new study, the researchers enrolled 2,120 women deemed to be of average risk for breast cancer. Women were excluded with any high-risk criteria, including personal or family history of breast cancer, history of tissue diagnosis associated with increased risk, and other factors. The women were randomized to undergo breast MRI and mammography screening every 12, 24, or 36 months.
There were a total of 3,861 completed screening rounds, covering a total of 7,007 woman-years. The mean age in the trial was 53.8 years.
Most of the MRI screens yielded a BI-RADS I or II finding (91%); 175 of the 3,861 screens were BI-RADS III, and after single MRI follow-up in 98.3% of those and biopsy in 1.7%, all 175 were uneventful/benign. Another 171 screens yielded a BI-RADs IV or V finding, and those women then underwent MR-guided biopsy.
Of that group, 39.8% were found to be benign; 35.7% were found to be malignant, and 24.6% were found to be high-risk (atypical ductal hyperplasia or lobular intraepithelial neoplasia). Kuhl said that this yielded a positive predictive value (PPV) of 60.5%, though the discussant for the session, A. Marilyn Leitch, MD, of the University of Texas Southwestern Medical Center, said that including the high-risk lesions in the calculation of PPV may not be appropriate. Without including those, the PPV was 35.7%.
Overall, there were 61 cancers detected in 2,120 women, for an overall detection rate of 28.8 per 1,000 women. Sixty of the 61 were only detected on MRI, and one was found on both mammography and MRI. The supplemental cancer yield of MRI in women undergoing mammography was 28.3 per 1,000 women, while the supplemental yield of mammography in women undergoing MRI was zero.
Twenty of the cancers (32.8%) were DCIS, and the other 67.2% were invasive; 42.6% of the cancers were high grade, and 32.8% were estrogen receptor (ER)/progesterone receptor (PR) negative. There were zero interval cancers discovered.
Kuhl concluded that MRI every 3 years could improve detection of some cancers in women at average risk. Leitch, though, pointed out that MRI false positive rates have been higher in other studies, and that the US Preventive Services Task Force has said that evidence is lacking on MRI as a replacement for mammography; she said that an updated version from USPSTF will likely have a similar finding. She advocated for a clinical trial comparing 3-year MRI with tomosynthesis mammography.