Mutation in Cutaneous Lymphoma Linked to Poor Prognosis
A new study confirms that patients with primary cutaneous diffuse large B-cell lymphoma who have a MYD88 mutation have a shorter disease-specific survival.
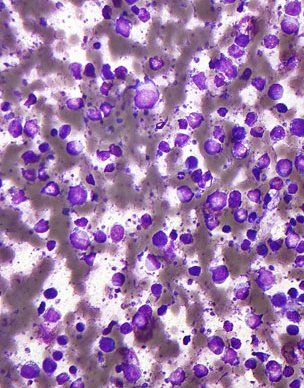
Micrograph of DLBCL, lymph node FNA specimen, field stain; source: Nephron, Wikimedia Commons
A new study confirms that patients with primary cutaneous diffuse large B-cell lymphoma, leg type (PCLBCL-LT) who have a MYD88 mutation have a shorter disease-specific survival compared with patients without the mutation.
Anne Pham-Ledard, MD, of Universitaire Bordeaux, Bordeaux, France, and colleagues confirmed this association in a retrospective multicenter study of medical records from 61 patients with PCLBCL-LT diagnosed between 1988 and 2010.
“Next-generation sequencing studies identified recurring and multiple genetic alterations implicated in the oncogenesis of nodal ABC-DLBCL, contributing to the nuclear factor-κB pathway constitutive activity,” Pham-Ledard and colleagues wrote in JAMA: Dermatology. “Notably, mutations affecting the B-cell receptor signaling pathway (CD79B) and other proteins affecting the nuclear factor-κB signaling most commonly, mutations of MYD88, CARD11, and TNFAIP3/A20 have been reported.”
Pham-Ledard sought to determine if any clinical features or outcomes were associated with MYD88 status. The median age of the patients examined was 79 years and 59% were women. Fifty-eight patients were ultimately included in the study group.
Results of the analysis showed that 59% of patients had the MYD88 L265P mutation. Although patients with and without the mutation had similar characteristics at presentation, those with the mutation were more likely to be older (P = .006), and had more frequent involvement of the leg (P = .008). No differences in sex, number of skin lesions, TNM stage at diagnosis, and treatment regimens were found.
Patients with the MYD88 mutation were also shown to have shorter 3-year (65.7% vs 85.4%) and 5-year specific survival rates (60.2% vs 71.7%) compared with patients with the wild-type allele.
In addition, patients with the mutations had a shorter disease-specific survival rates in both univariate (P = .03) and multivariate analysis (P = .02).
“Mutation of MYD88 predicts a poorer outcome considering MYD88 signaling and nuclear factor-κB pathway activation as actionable targets,” the researchers wrote. “Therapeutic strategies targeting either B-cell receptor signaling (as ibrutinib, the Bruton tyrosine kinase inhibitor, or fostamatinib targeting the spleen tyrosine kinase), or the interferon regulatory factor-4 and the transcription factor Spi-B (targeted by lenalidomide), or NF-κB proteasome inhibitor (bortezomib), or MYD88 inhibitors, seem promising in ABC-DLBCL and especially in PCLBCL-LT.”