Natural Killer Cells Could Fight Off ALL
A laboratory study found that natural killer cells could be multiplied from the blood of patients to fight off precursor B-lineage acute lymphoblastic leukemia.
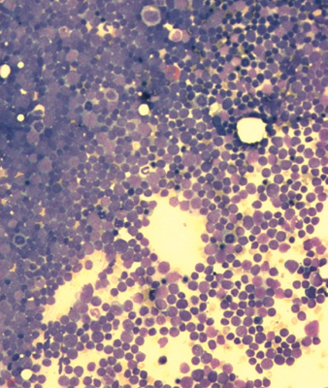
Bone marrow smear from a patient with ALL; source: Furfur, Wikimedia Commons
A laboratory study found that CD56+ immune effector cells, or natural killer cells, could be multiplied from the blood of patients with precursor B-lineage acute lymphoblastic leukemia (pre-B ALL), and that those natural killer (NK) cells could be an effective tool in fighting off the malignancy without the risks associated with donor-based immunotherapy.
Patients with pre-B ALL typically have “a marked perturbation of normal hematopoiesis,” according to study authors led by Nora Heisterkamp, PhD, of the University of Southern California, meaning a deficiency in NK cells could contribute to the cancer’s progression. While donor cells could fight off the disease, there is a serious risk of graft-vs-host disease; the current study was designed to see if a patient’s own cells could be expanded to avoid that risk and help treat the ALL. The results were published online ahead of print on August 19 in Leukemia.
The group was able to expand CD56+ cells from both bone marrow and from peripheral blood samples, and from both newly diagnosed patients and from relapse samples as well. They then tested those cells for cytotoxic activity against ALL cells, and found such activity to be similar to normal NK cells derived from peripheral blood mononuclear cells.
And importantly, the CD56+ cells have specifically autologous activity. The cytotoxicity seen in the study could be improved further by the addition of interleukin-15; when cultured with IL-15 overnight the improvement was greatest.
The authors noted that if CD56+ lymphocytes could be expanded to sufficiently useful numbers then this treatment could be ready for use almost immediately. Though it is unclear at present exactly how many cells are needed, the authors were confident that enough cells could be generated from most patients with pre-B ALL.
“In this study, we used NK cells and ALL cells from the same pediatric patients,” Heisterkamp said in a press release. “We found that autologous natural killer cells will destroy the patient's leukemia cells.” Her co-lead investigator, Hisham Abdel-Azim, MD, of Children’s Hospital of Los Angeles, added that the results are very promising and that the treatment could particularly be used following chemotherapy as a way to ensure the eradication of minimal residual disease. “We anticipate additional pre-clinical testing, and then a clinical trial to evaluate the therapy in children with leukemia,” he said.