Nearly One-Fifth of Screened Lung Cancer Cases May Be Indolent
An analysis of data from the National Lung Screening Trial found that more than 18% of all lung cancers detected through low-dose CT screening were indolent.
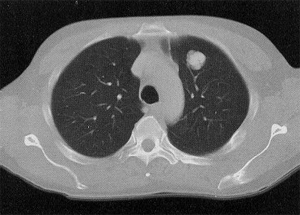
A single CT slice at the level of the aortic arch demonstrates a lobulated, 3-cm left upper lobe adenocarcinoma
An analysis of data from the National Lung Screening Trial (NLST) found that more than 18% of all lung cancers detected through low-dose computed tomography screening were indolent, with even higher rates for certain subtypes of cancer. In spite of this apparently potential harm related to screening, the US Preventive Services Task Force recently endorsed a screening program for high-risk individuals.
The new study, led by Edward F. Patz Jr, MD, of Duke University Medical Center in Durham, North Carolina, was published in December in JAMA Internal Medicine. The analysis included results of the NLST involving 53,452 individuals with at least a 30 pack-year smoking history. It found that among the 1,089 lung cancers detected in the low-dose CT arm of the NLST, the probability of an overdiagnosed case was 18.5%.
Specifically among non–small-cell lung cancer (NSCLC) cases, the probability of an overdiagnosis was 22.5%. Most strikingly, the probability of a bronchoalveolar lung cancer overdiagnosis was 78.9%. The original NLST analysis, which found a 20% reduction in lung cancer mortality with low-dose CT screening over chest radiography, determined that 320 patients needed to be screened to prevent one cancer death; this analysis showed that among those 320 screened to prevent a death there would need to be 1.38 cases of overdiagnosis.
Overdiagnosis, which essentially means that a cancer found on screening is so slow-growing that treatment would likely not be needed, represents a significant harm to be included in cost-benefit analyses of screening programs. In the recent USPSTF recommendations for such a program, the task force noted an extremely high rate of false positives with low-dose CT-more than 95%-but suggested that only 10% to 12% of screening-detected cancers are overdiagnosed.
An indolent tumor found on low-dose CT screening could result in invasive and toxic treatments that would otherwise have not been necessary, given that indolent cases are essentially impossible to distinguish from others at first glance. And even if methods to remedy that issue are developed, explaining to a patient that a lung cancer case does not require treatment represents an extremely difficult problem for physicians.
The authors of the new study noted that this particular model includes only three annual screenings and a total of about 7 years of follow-up. “Therefore, the estimates of true overdiagnosis, based on the lifetime follow-up scenarios, must be treated cautiously,” they wrote. “In the future, once there are better biomarkers and imaging techniques to predict which individuals with a diagnosis of lung cancer will have more or less aggressive disease, treatment options can be optimized, and a mass screening program can become more valuable.”