Neoadjuvant Regimen Ups Response Rates in Triple-Negative Breast Cancer
Adding either carboplatin or bevacizumab to a neoadjuvant regimen increased rates of pathologic complete response in triple-negative breast cancer patients.
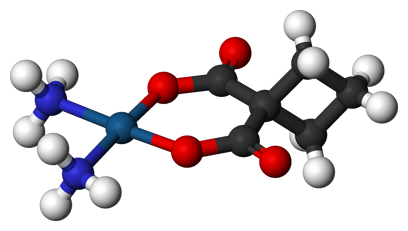
Ball-and-stick model of carboplatin.
The addition of either the chemotherapy carboplatin or the angiogenesis inhibitor antibody bevacizumab to a standard neoadjuvant treatment regimen significantly increased the rates of pathologic complete response (pCR) in triple-negative breast cancer (TNBC) patients with stage II/III disease. Still, the study authors could not definitively conclude that these combinations improve overall survival or relapse-free survival. The final results of the Cancer and Leukemia Group B (CALGB) 40603 trial were published in the Journal of Clinical Oncology.
The preliminary results were presented at the 2013 San Antonio Breast Cancer Symposium last December.
In this final analysis, it was shown that the addition of carboplatin resulted in a 60% pCR rate in the breast compared with 44% with the standard chemotherapy backbone of paclitaxel plus doxorubicin and cyclophosphamide (P = .0018). Adding bevacizumab resulted in a 59% pCR rate in the breast compared with 48% with the chemotherapy backbone alone (P = .0089). According to the study authors, adding either carboplatin or bevacizumab to the neoadjuvant regimen did not result in more than an additive effect.
The addition of carboplatin (but not bevacizumab) increased the pCR rates in the breast and axilla by 54% in those patients who were treated with the combination compared with 41% in those treated with the chemotherapy backbone regimen alone (P = .0029).
The study included 443 patients with stage II or III TNBC. All patients received the standard neoadjuvant chemotherapy backbone of once weekly 80 mg/m2 paclitaxel for 12 weeks, followed by doxorubicin combined with cyclophosphamide once every 2 weeks for 4 cycles. Patients were randomized to receive either only the backbone therapy or one of a few combinations-additional carboplatin, additional bevacizumab, or both carboplatin and bevacizumab. Concurrent carboplatin was administered once every 3 weeks for 4 cycles, and bevacizumab was administered at 10 mg/kg once every 2 weeks for 9 cycles.
Most of the patients on the study were between the ages of 40 and 59 years.
Because TNBC is defined more by its lack of molecular abnormalities, there are currently no targeted therapies for this disease, which remains to be better defined. The standard treatment for TNBC is chemotherapy, and the prognosis for TNBC remains worse compared to other breast cancer subtypes.
Patients in the experimental arms were more likely to stop treatment due to toxicity compared with those in the standard treatment control arm. Six percent (7 patients) in the carboplatin-only arm and 12% (26 patients) in the bevacizumab arm, with or without carboplatin, stopped treatment early. Due to toxicities and treatment delay, only 80% of carboplatin-assigned patients completed all 4 doses and only 66% of patients in the bevacizumab arms received all 9 doses. Only one patient in the control arm discontinued therapy due to toxicity; six patients stopped early due to disease progression.
The addition of carboplatin to the chemotherapy backbone increased grade 3, 4 neutropenia, febrile neutropenia, leukopenia, and thrombocytopenia. Patients who received bevacizumab were more likely to develop grade 3 hypertension compared with those who did not receive bevacizumab (12% in the bevacizumab arm, 10% in the bevacizumab plus carboplatin arm, and 2% and 0% in the control and carboplatin arms, respectively). One on-study death was linked to uncontrolled hypertension.
“Results from CALGB 40603 and other studies justify consideration of definitive trials to determine whether inclusion of carboplatin leads to improvements in long-term outcomes in early-stage TNBC, preferably limited to biologically defined patient subsets believed most likely to benefit from this treatment,” concluded the authors.