New Anti-Cancer Agent Developed for HER2-Positive Breast Cancer Shows Promise in Pre-Clinical Studies
Scientists at the NCI have designed a novel protein, HER2-Affitoxin, aimed to treat HER2-positive breast cancer. In vitro experiments and mouse breast cancer models show that the agent is highly effective in eradication of HER2-over expressing cancer cell as well as tumors in mice.
Scientists at the NCI have designed a novel protein, HER2-Affitoxin, aimed to treat HER2-positive breast cancer. In vitro experiments and mouse breast cancer models show that the agent is highly effective in eradication of HER2-over expressing cancer cell as well as tumors in mice. The results of the research are published today, July 26, 2011, in Clinical Cancer Research (doi: 10.1158/1078-0432.CCR-10-2887).
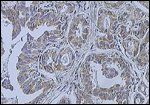
Breast cancer (Infiltrating ductal carcinoma of the breast) assayed with anti HER-2 (ErbB2) antibody; source: Wikimedia Commons user Itayba
Jacek Capala, PhD, DSc, lead author of the study, and colleagues at the NCI designed and produced HER2-Affitoxin, which consists of an HER2-specific antibody linked to PE38, a modified bacterial toxin, that causes cell death by blocking protein translation. HER2-Affitoxin is an immunotoxin/affibody that is able to selectively bind to cancer cells overexpressing HER2. The mechanism of targeted-cell killing is likely an internalization of a fraction of the HER2-Affitoxin into the cytosol of the cell whereupon the PE38 toxin portion of the molecule blocks enzymatic activity of protein crucial for protein synthesis and kills the cell.
The goal was to create a novel treatment for breast cancers that overexpress HER2 but that acquires resistance to standard treatments such as trastuzumab. Trastuzumab is an effective monoclonal antibody that binds and interferes with the HER2 receptor and is used to treat HER2-overexpressing breast cancer. Unfortunately, a subset of patients does not respond or acquires resistance to the treatment, creating an unmet need for this patient population.
HER2 is overexpressed in other cancers such as non–small lung carcinoma, ovarian carcinomas and B-cell acute lymphoblastic leukemia. Combined with breast cancer, HER2-amplified cancers account for 20% of all of these cancers combined. HER2 overexpression, particularly in breast cancer, is associated with a more aggressive form of cancer that has an unfavorable prognosis. While trastuzuman has changed the prognosis of many HER2-positive breast cancer patients, a subset of these patients represents an unmet need for treatment.
“Unlike the current HER2-targeted therapeutics such as Herceptin, this protein does not interfere with the HER2 signaling pathway but, instead, uses HER2 as a target to deliver a modified form of bacterial toxin specifically to the HER2-positive cancer cells. When cells absorb the toxin, it interferes with protein production and, thereby, kills them,” said Capala.
The current study analyzed the in vivo characteristics of HER2-Affitoxin including pharmacokinetics and biodistribution analyses that showed fluorescently labeled HER2-Afflitoxin in the kidneys, liver, and a “significantly lower but still over-the-background signal” in mouse tumors. Efficacy experiments using mouse models with HER2-positive breast tumors showed tolerable treatment and an average of 60% reduction in tumor size 3 days after the first injectible dose. The tumors remained 5% of their size prior to treatment and did not regrow after 76 days post-first treatment. Notable, even relatively large and aggressive tumors stopped growing and most disappeared. This effect, according to Professor Capala, justifies moving the compound into first in-human clinical trials.
“The fact that a dose as low as 0.1 mg/kg was enough to eradicate relatively large tumors, with only mild toxicity observed at higher doses, suggests a therapeutic window broad enough to provide effective and safe treatment of HER2-positive tumors,” according to the article.
The immunogenicity of the agent was tested in order to assess the immunological reaction that will occur with longer-term treatment. HER2-Affitoxin induced a humoral but not a cellular-mediated immune response and anti-HER2-Affitoxin antibodies were detected in mice. According to the authors, efforts to improve the therapeutic potency of this agent will continue as an antibody response may result in neutralization of the agent in the body, limiting its effectiveness with multiple rounds of treatment.
Whether in-human trials will begin following more characterization pre-clinical studies is still an open question, however. First in-human trials would test repeated treatments and immnugenicity reactions as well as the effect of HER2-Affitoxin on normal tissues that express HER2 at a low level, according to Professor Capala.
“As a translational researcher focusing on pre-clinical studies, I did all I could to show the potential of Affitoxin. I have also developed and validated in pre-clinical studies an Affibody based HER2-imaging agent that might be used for in vivo assessment of HER2 expression before and during HER2-targeted therapies I do my best to get clinicians interested in this approach,” says Capala.
Professor Capala and his translational research colleagues at the NCI have laid the groundwork of preclinical data for HER2-Affitoxin. At this point, subsequent characterization and human trials will be up to a company or other institution to take over. “The high affinity and specificity of this Affitoxin to HER2 is due to it’s targeting moiety HER2-specific Affibody molecule, which I received through a Collaborative Research and Development Agreement (CRADA) with a Swedish company, Affibody AB, Stockholm. I have sent them all my research materials resulting form this CRADA, including HER2-Affixotin, and I hope that either this company or one of their other collaborators would like to continue the projects I initiated at NCI” voiced Professor Capala.
“Herceptin has been very successful in improving the treatment outcome for HER2-positive breast cancer. However, currently there are limited therapeutic options for HER2 positive tumors that either do not respond or develop resistance to it. Obviously, since there is a need for a new treatment for those patients, they could benefit most form HER2-Affitoxin and, consequently, it should be tested first in this patient population,” says Jacek Capala. “Affitoxin could offer another therapeutic option for those patients whose tumors no longer respond to Herceptin.”