New Breast Screening Technology Can Increase Accuracy of Diagnosis
A new study shows that adding a new three-dimensional breast imaging technique called tomosynthesis to digital mammography can increase diagnostic accuracy and reduce false-positive rates.
A new study shows that adding a new three-dimensional breast imaging technique called tomosynthesis to digital mammography can increase diagnostic accuracy and reduce false positive rates. The 1,192-patient study is published in Radiology. The study compared tomosynthesis in combination with mammography compared to mammography alone.
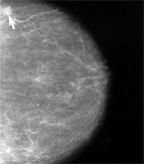
Standard mammography showing a small cancerous lesion (arrow); a new study found that adding tomosynthesis to digital mammography was more accurate than mammography alone
Elizabeth A. Rafferty, MD, of the department of radiology at Massachusetts General Hospital in Boston, and colleagues recruited women from five sites. All 27 radiologists had increased diagnostic accuracy when tomosynthesis was added to the analysis-false positive rates decreased with the diagnostic combination (P < 0.03). The highest increase in sensitivity was for invasive cancer cases.
Tomosynthesis can both reduce false positive rates and can facilitate finding cancers that may be missed by standard mammograms, said Rafferty. As many as 30% of breast cancers are not detected by mammograms, according to previous studies. High breast density is one reason for a mammogram false negative.
Breast tomosynthesis is a digital technique that produces two x-ray images of each breast. Multiple, low-dose images from different angles are produced for each breast and reconstructed, increasing sensitivity and specificity of the image. The radiation dose for the procedure is 3 mGy, the radiation exposure limit for a single mammogram, according to the US Food and Drug Administration (FDA). Unlike standard mammography where a two-dimensional image of the breast is used for diagnosis and can prevent views of specific areas, tomosynthesis (approved by the FDA in February of 2011) is a three-dimensional technique that can improve visualization.
Compared to a mammogram alone, the combination of mammogram and tomosynthesis increased diagnostic accuracy by 10.7% for one set of radiologists in the study, and by 16% in the second set. All 27 radiologist reviewers improved their diagnostic accuracy, according to the study. All of the readers also showed a significant decrease in their noncancer recall rates. “Clinically, such a reduction in recall rate can be expected to translate to a substantial number of unnecessary diagnostic tests being avoided,” the authors stated in the discussion of their results. Reducing the number of false positives would not only lower clinical costs, but save women from the emotional stress of receiving a positive diagnosis.
The authors note that there are limitation to reader-type studies compared to a true screening population. Clinical screening studies are needed to confirm these results.
Combining these two techniques provides an advantage: a standard mammogram allows the radiologist to compare the current image with previous ones and to analyze different tissue aspects while tomosynthesis allows for better visuals of the tissue features not well-seen by mammograms. The radiation exposure is higher with this combined technique, however.
The vast majority of the increase in sensitivity of diagnosis with the combined mammogram and tomosynthesis technique was due to the improved detection of invasive cancers, said Rafferty in a press release. The reduction in false positive rates, according to Rafferty, would be expected to translate into a substantial reduction in unnecessary diagnostic tests.