New Prostate Cancer Test Gets FDA Approval
A new noninvasive blood test for prostate cancer detection won the approval of the FDA last month. The manufacturer believes the test will provide better detection and a decrease in costs.
A new noninvasive blood test for prostate cancer detection won the approval of the US Food and Drug Administration (FDA) on June 25, 2012. The company that makes the test, Beckman Coulter, believes that their Prostate Health Index (PHI) will not only provide better detection, but also decrease costs. The new test will be available in the United States starting this summer.
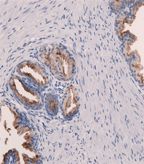
Immunohistochemistry of prostate specific antigen in normal prostate glands; source: Jensflorian, Wikimedia Commons
The company conducted a pivotal trial comparing their test to the standard prostate-specific antigen (PSA) currently used to detect prostate cancer, finding a 2.5-fold increase in specificity with the new test compared to the PSA test when patients had PSA values in the range of 4 ng/ml to 10 ng/ml-just the upper limit of what are considered normal PSA levels. The trial demonstrated a 31% reduction in the number of negative biopsies among patients with a positive blood test compared to those screened with a standard PSA assay.
The PHI test measures three components (PSA, free PSA, and a PSA precursor form [-2]pro-PSA) and from these three metrics, the probability of prostate cancer is calculated and used to help distinguish between a benign prostate condition that results in elevated PSA levels and prostate cancer that may require treatment. The test is aimed for men with PSA levels between 2 ng/ml and 10 ng/ml and a normal digital rectal exam.
Beckman Coulter believes that the new test will help address the recent PSA testing controversy. The US Preventive Services Task Force issued a a statement in May 2012 that the majority of men are harmed as a result of prostate cancer screening, having weighed screening and prevention with the overdiagnosis and overtreatment of slow-growing prostate cancer. The harms include mental stress related to a positive diagnosis, and invasive biopsies that can result in fever, infection, and urinary issues. Members of the task force stated that the number of men who do not die of prostate cancer due to screening over a period of 10 to 14 years is small. The task force indicated that better testing and treatment options are necessary, recommending against regular PSA-based screening for those men with no symptoms of prostate cancer.
A cost-effectiveness analysis published at the end of last year compared the new test to the standard PSA screening, concluding that the combination of the PHI and standard PSA screening test is both cost-effective and is a better combined tool for recommendation of a prostate biopsy.
More data is still needed, however to understand whether this new test will be able to better distinguish between prostate cancer that requires treatment and slow-growing prostate cancer that can be monitored by so-called “active surveillance.”
Reference
1. Nichol MB, Wu J, Huang J, et al. Cost-effectiveness of Prostate Health Index for prostate cancer detection. BJU Int. 2011 Nov 11. [Epub ahead of print]