New Way to Target B-Cell Lymphomas
Researchers at the University of Pennsylvania have identified a protein that could be targeted to turn off B-cell lymphomas. The protein, CD19, was found to be a major regulator of B-cell neoplastic growth driven by the MYC oncogene.
Researchers at the University of Pennsylvania have identified a protein that could be targeted to turn off B-cell lymphomas. The protein, CD19, was found to be a major regulator of B-cell neoplastic growth driven by the MYC oncogene.
The research could lead to an approach to specifically target a subset of lymphomas, according to the lead study author, Andrei Thomas-Tikhonenko, PhD, an oncology researcher at the Children’s Hospital of Philadelphia and associate professor at the University of Pennsylvania School of Medicine. The study shows a key biological pathway that leads to B-cell lymphoma-and the potential to break the addiction of these cancer cells. The research is published in the Journal of Clinical Investigation.[1]
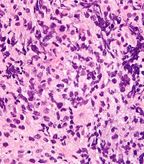
Very high magnification micrograph of a primary mediastinal large B-cell lymphoma; source: Nephron, Wikimedia Commons
A high level of MYC protein correlates with high levels of the CD19 protein. Thomas-Tikhonenko et al have uncovered a previously unknown molecular pathway that depends on CD19, implicating the protein as an on-off switch in this pathway.
B-cell lymphomas include both Hodgkin lymphomas and non-Hodgkin lymphomas. Oncogenic addiction is particularly relevant in blood cancers in which tumor growth is supported by a lower frequency of driver mutations. One of these drivers is the c-MYC protein that is mutated in both Burkitt lymphoma as well as some diffuse large B-cell lymphomas (DLBCL). A second transcription factor involved in B-cell lymphoma development is paired box transcription factor 5 (PAX5), also implicated in B-cell lineage leukemias and lymphomas through its role in B-cell receptor signaling. There is mouse model data that suggests that both c-MYC and B-cell receptor signaling are involved in B-cell lymphomagenesis. Whether MYC and PAX5 directly interact to drive the cancer was previously unclear.
This study now shows that both PAX5 and its downstream target, CD19, regulate MYC protein levels through a post-transcriptional mechanism. When expressed at high levels, MYC, a transcription factor, causes uncontrolled cell growth and tumor development. CD19 is a cell surface receptor on B cells. CD19 signaling functions to activate the PI3K pathway in the context of B-cell receptor (BCR) signaling for expansion of B cells. Using both in vivo and in vitro models, the new research now shows that CD19 also functions independent of BCR to regulate MYC levels through the PI3K pathway. “This was a complete surprise to immunologists here at Penn,” said Thomas-Tikhonenko.
“We found that CD19 is absolutely required to stabilize the MYC protein,” explained Thomas-Tikhonenko. “Basically, the more MYC protein and the more stable it is, the more likely a lymphoma patient will have a poor prognosis.”
Thomas-Tikhonenko and colleagues also analyzed MYC and CD19 expression in DLBCL patients. They found that high expression of either gene correlated with negative effects on patient survival.
While the expected and typical result that blocking an important driver pathway results in activity of a compensatory pathway, in this case there is no such pathway, according to Thomas-Tikhonenko. “Without CD19, there is no MYC,” he added, “so controlling that on-off switch could represent a powerful tool against lymphoma.”
The Results Can Help Design Better Targeted Lymphoma Therapies
Current clinical trials are testing anti-CD19 antibodies in lymphoma patients. One of these antibodies is ImmunoGen’s SAR3419 that has shown favorable activity in B-cell non-Hodgkin lymphoma in a phase I trial. A phase II trial testing the drug as a monotherapy in relapsed or refractory DLBCL patients is currently recruiting patients. The drug is also in a phase II trial in combination with rituximab.
The issue with CD19 targeted antibodies, according to Thomas-Tikhonenko, is that they attack all B cells nonselectively, weakening the immune system. The data from the University of Pennsylvania suggests that a way to target only the cancerous B cells has been identified. “Current anti-CD19 and anti-CD20 antibodies wipe out all [of the patient’s B cells], normal and malignant, leaving the patient without humoral immunity,” explained Thomas-Tikhonenko. “The idea is that if we could target the CD19–PI3K interaction, this treatment might spare normal B cells in which MYC protein levels are low.”
Future Steps
Thomas-Tikhonenko’s laboratory is studying alternative growth pathways in various B-cell neoplasms to identify new therapy approaches. “We have some interesting preliminary data that suggest CD19 mutants unable to engage PI3K still promote tumor growth, albeit less effectively,” said Thomas-Tikhonenko. The researchers also plan to examine pediatric lymphomas for the CD19 and MYC protein level correlation.
In the long-term, Thomas-Tikhonenko and colleagues hope to ultimately take their findings to the clinic, but for now will test currently available anti-CD19 antibodies, including the one from MedImmune in their in vivo models.
Reference
1. Chung EY, Psathas JN, Yu D, et al. CD19 is a major B cell receptor-independent activator of MYC-driven B-lymphomagenesis. J Clin Invest. 2012 May 1. [Epub ahead of print]