Advances in our understanding of the molecular pathogenesis of B-cell lymphoma have guided the development of targeted therapies that disrupt aberrant signaling pathways important for communication within lymphoma cells and for their interactions with the tumor microenvironment. This has led to unprecedented therapeutic progress, with biologic agents that have begun to transform the care of patients with lymphoma and chronic lymphocytic leukemia. This review discusses the mechanisms of action, clinical development, and emerging applications of small-molecule inhibitors that target B-cell receptor signaling pathways, B-cell lymphoma-2 inhibitors, selective inhibitors of nuclear export, and epigenetic modifiers.
Introduction
Combination immunochemotherapy has been the traditional treatment framework for patients with B-cell lymphoma/chronic lymphocytic leukemia (CLL). It is delivered as an infusional treatment for a finite period; the intensity and frequency of therapy are limited by myelosuppression and its associated morbidities. With the exception of aggressive subtypes such as diffuse large B-cell lymphoma (DLBCL), most indolent subtypes (including follicular lymphoma [FL] and CLL/small lymphocytic lymphoma [SLL]) and mantle cell lymphoma (MCL) remain incurable following immunochemotherapy.
Relapsed disease from both aggressive and indolent subtypes is often resistant to chemotherapy and requires novel treatment. Therefore, biologic agents without the typical adverse effects of chemotherapy hold great promise for patients with comorbidities who are intolerant of chemotherapy, and for those with relapsed/refractory B-cell lymphoma/CLL. Studies of small-molecule inhibitors that target B-cell receptor (BCR) pathways-namely Bruton tyrosine kinase (BTK) inhibitors and phosphoinositide 3-kinase (PI3K) inhibitors-as well as B-cell lymphoma-2 (BCL-2) inhibitors, have demonstrated unprecedented clinical benefit; optimal treatment duration and combinations are under active investigation. However, the novel mechanisms of action of these agents have presented challenges, including measurement of responses, management of adverse effects, and detection of potential resistance mechanisms.
BTK Inhibitors
Mechanism of action
BCR signaling promotes cell survival and lymphomagenesis in a number of B-cell malignancies, including CLL, MCL, FL, Waldenström macroglobulinemia (WM), and DLBCL.[1] BTK, a member of the Tec kinase family and a critical cytoplasmic mediator of the BCR signaling cascade, is a uniquely attractive target for selective B-cell inhibition. The first-in-class small-molecule BTK inhibitor ibrutinib is an irreversible and selective oral drug that covalently binds to cysteine-481 near the adenosine triphosphate–binding domain of BTK, with an IC50 of 0.5 nM. Blockage of BCR signaling via BTK inhibits phospholipase (PL) C γ2 phosphorylation; nuclear factor kappa B (NF-kB) activation; and downstream signaling for proliferation, migration, and adhesion. This leads to a reduction of lymphadenopathy that can be accompanied by transient redistribution lymphocytosis.[2] Second-generation BTK inhibitors (eg, acalabrutinib [ACP-196] and BGB-3111) aim to provide greater target specificity and potency with reduced off-target inhibition.
Clinical applications of ibrutinib
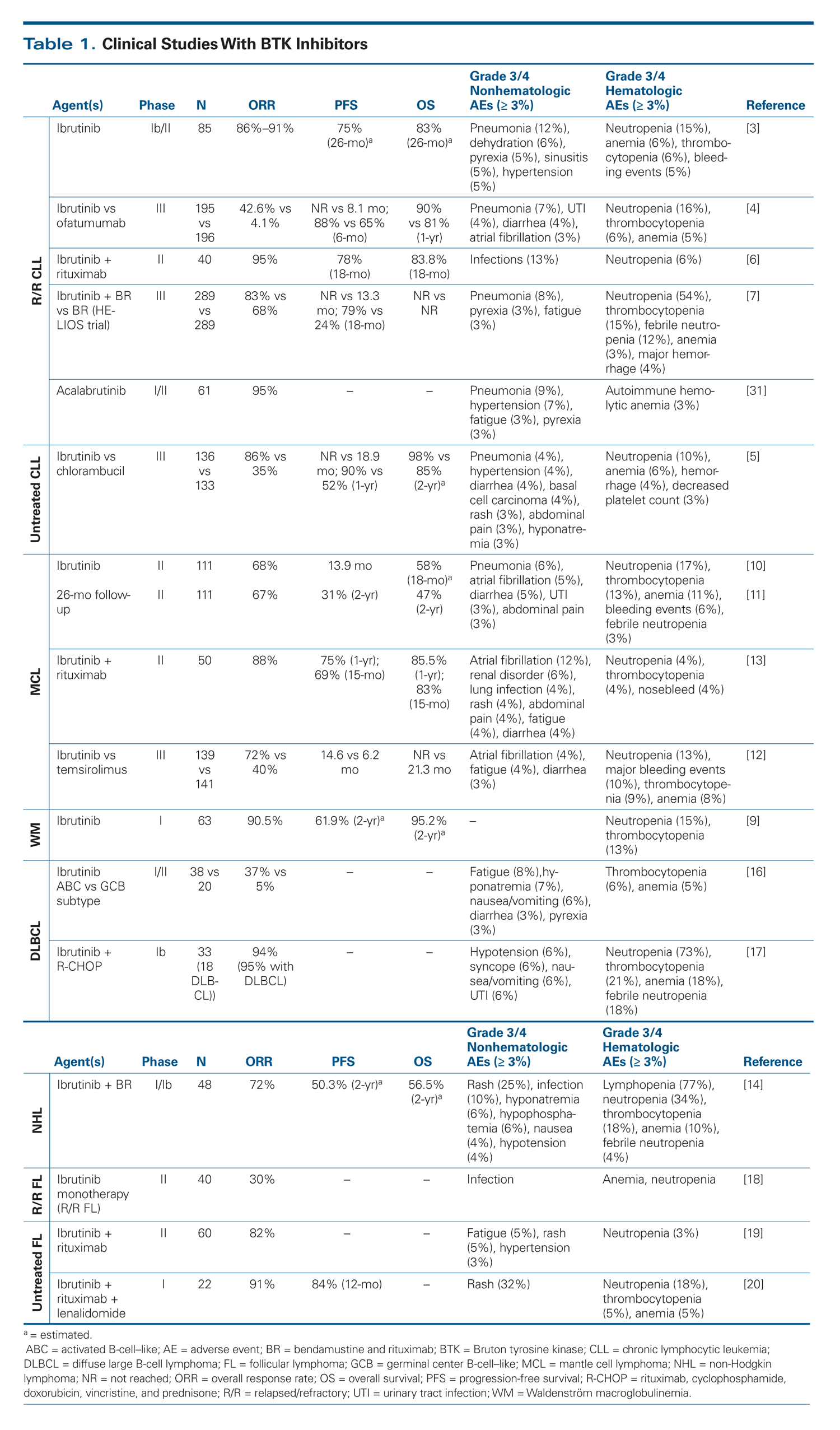
Ibrutinib received accelerated approval from the US Food and Drug Administration (FDA) for relapsed/refractory MCL in November 2013 and for relapsed/refractory CLL in February 2014. The indication for CLL was expanded to include patients with 17p deletion in July 2014, and ibrutinib received approval as first-line therapy for treatment-naive patients in March 2016. It was approved in January 2015 for patients with WM. Combination regimens that include ibrutinib and second-generation BTK inhibitors are in various stages of clinical development; the highlights are summarized according to disease subtypes in Table 1.
Ibrutinib in CLL. In the first phase Ib/II trial, Byrd et al studied the safety and efficacy of ibrutinib in 85 patients with relapsed or refractory CLL, including 65% with advanced-stage disease, 33% with 17p13.1 deletion, and 36% with 11q22.3 deletion.[3] Ibrutinib was provided at a daily dose of either 420 mg (51 patients) or 840 mg (34 patients); treatment continued until disease progression or unacceptable toxicity occurred.
The overall response rate (ORR) was 71%, with an additional 15% to 20% experiencing a partial response (PR) with lymphocytosis, independent of dose levels, clinical features, and cytogenetic risk factors. Progression-free survival (PFS) at 26 months was 75% and overall survival (OS) was 83%; PFS and OS were decreased, at 57% and 70%, respectively, in those with 17p13.1 deletion. Adverse events were mild to moderate, including grade 1/2 nonhematologic toxicities such as diarrhea, fatigue, infections, and rash. Grade 3/4 bleeding was reported in 4 patients. Grade 3/4 hematologic toxicity was infrequent. In view of the high response rates, ibrutinib at 420 mg/d was given accelerated approval by the FDA in February 2014.
The phase III RESONATE study randomized 391 patients with previously treated CLL to either ibrutinib or the anti-CD20 antibody ofatumumab, with crossover allowed for the ofatumumab arm.[4] Ibrutinib significantly improved the duration of PFS: not reached vs 8.1 months in the ofatumumab arm (P < .001) at a median follow-up of 9.4 months. At 12 months, ibrutinib had superior OS (90% vs 81% in the ofatumumab group; P = .005) and ORR (42.6% vs 4.1%; P < .001). Those patients with a 17p13.1 deletion had a markedly improved duration of PFS with ibrutinib: not reached compared with 5.8 months with ofatumumab. Ibrutinib was associated with a slightly increased risk of grade 3/4 diarrhea (4% vs 2%) and atrial fibrillation (3% vs 0%) compared with ofatumumab, which had not previously been well recognized. The rate of bleeding-related adverse events, including petechiae and ecchymoses, was higher in the ibrutinib arm (44%) than in the ofatumumab arm (12%), although rates of major hemorrhage were not significantly different. Based on the evidence of risk reduction in both PFS and OS, the FDA expanded the approval of ibrutinib to include treatment of CLL patients with 17p deletion.
The phase III RESONATE-2 study went on to compare ibrutinib with the standard of care, first-line chlorambucil, in 269 patients aged ≥ 65 years with previously untreated CLL.[5] At a median follow-up period of 18.4 months, the primary endpoint, PFS, was not reached in the ibrutinib arm compared with 18.9 months in the chlorambucil arm. OS at 24 months was 98% with ibrutinib vs 85% with chlorambucil. These results equaled an 84% risk reduction for progression or death. In addition, the ORR was higher with ibrutinib than with chlorambucil (86% vs 35%; P < .001). Grade 3 diarrhea (4%) and atrial fibrillation (6%) were more frequent with ibrutinib, as was grade 3/4 hemorrhage (4% vs 2% with chlorambucil). The results of this trial established the use of ibrutinib as a first-line agent in CLL.
Emerging ibrutinib combinations have been explored in CLL. The combination of rituximab with ibrutinib (iR) was studied in 40 patients with high-risk CLL; the trial demonstrated an ORR of 95%, an 18-month PFS of 78%, an 18-month OS of 83.8%, and an early clearance of redistribution lymphocytosis compared with single-agent ibrutinib.[6] The ongoing randomized trial of ibrutinib vs iR (ClinicalTrials.gov identifier: NCT02007044) will further define the role of rituximab in the combination. The phase III HELIOS trial compared outcomes when ibrutinib was added to the standard bendamustine and rituximab (BR) combination (iBR) in 578 patients with relapsed/refractory CLL. An interim analysis demonstrated that the addition of ibrutinib improved outcomes: 18-month PFS was 79% in the iBR group compared with 24% in the BR group.[7] Minimal residual disease was also significantly decreased with ibrutinib (42%) compared with placebo (20%). Adverse events were generally comparable and expected. Numerous other studies with ibrutinib chemoimmunotherapy combinations are ongoing: examples include iBR in elderly patients with previously untreated CLL (NCT01886872); ibrutinib, fludarabine, cyclophosphamide, and rituximab (iFCR) in younger patients with previously untreated CLL (NCT02251548); and ibrutinib in combination with obinutuzumab-based regimens (NCT02264574, NCT02537613, and NCT02629809).
Ibrutinib in WM.MYD88 L265P mutation-which activates NF-kB through BTK and interleukin-1 receptor–associated kinase (IRAK) 1 and IRAK4 and can be targeted by ibrutinib-is the most prevalent mutation in WM; it affects 93% to 97% of patients.[8] The presence of the CXCR4 WHIM (warts, hypogammaglobulinemia, immunodeficiency, myelokathexis) mutation in WM patients who have the MYD88 L265P variant confers resistance to ibrutinib. These findings prompted a multicenter clinical trial of ibrutinib monotherapy at 420 mg daily in patients with previously treated WM to assess response.[9] Of the 63 patients enrolled, the MYD88 L265P mutation was present in 89% and the CXCR4 WHIM mutation in 34%. The ORR was 90.5%, and the major response rate was 73%. Response rates were highest in the MYD88 L265P/CXCR4 wild-type group (100%) followed by the MYD88 L265P/CXCR4 WHIM group (85.7%) and the MYD88 wild-type/CXCR4 wild-type group (71.4%). The estimated 2-year PFS was 69.1% and OS was 95.2%. The adverse events were consistent with those reported in previous studies of ibrutinib monotherapy. Based on the durable responses, the FDA approved ibrutinib for the treatment of WM in January 2015.
Ibrutinib in MCL. Constitutive activation of BCR signaling is essential for the growth of MCL cells. Wang et al reported the results of an international open-label phase II study of ibrutinib monotherapy at a dose of 560 mg daily in 115 patients with relapsed/refractory MCL who had received a median of three prior therapies.[10,11] At a median follow-up of 26.7 months in 111 evaluable patients, the ORR was 67%, with 23% experiencing a complete response (CR). The median time to CR was 5.5 months, with a duration of response of 17.5 months. The PFS was 13 months, and the median OS was 22.5 months. The 2-year PFS and OS were 31% and 47%, respectively. The most common adverse events were diarrhea (54%), fatigue (50%), nausea (33%), and dyspnea (32%). Grade ≥ 3 bleeding included hematuria (2%) and subdural hematoma (2%). Twelve patients (11%) reported atrial fibrillation, with a mean time to onset of 140 days. In November 2013, the FDA granted accelerated approval to ibrutinib for the treatment of patients with relapsed/refractory MCL.
A subsequent randomized phase III clinical trial led by the European MCL Network compared ibrutinib with temsirolimus, an approved second-line therapy in the European Union, in patients with relapsed/refractory MCL.[12] The primary endpoint of the study was PFS. A total of 280 patients were randomized to receive either a daily oral 560-mg dose of ibrutinib or intravenous temsirolimus. Ibrutinib outperformed temsirolimus in both PFS (14.6 months vs 6.2 months) and ORR (72% vs 40%) and was better tolerated. The response rate for subsequent treatment was similar between the two arms at 20%. The reported adverse events were consistent with previous studies, including atrial fibrillation (4% with ibrutinib vs 1% with temsirolimus) and major bleeding (10% with ibrutinib vs 6% with temsirolimus).
Ibrutinib combination regimens are being actively explored in MCL. Wang et al reported the results of a study of iR in 50 patients with relapsed MCL.[13] The ORR was 88%, with CRs in 44%. Patients with Ki-67 levels of < 50% achieved a 100% ORR, with median duration of response, PFS, and OS not reached. The ORR was significantly lower-at 50%, with CRs in 17%-in patients with Ki-67 levels of ≥ 50%. Maddocks et al studied the combination of iBR in 48 patients with non-Hodgkin lymphoma (NHL), including 17 with untreated or relapsed/refractory MCL.[14] Patients received 6 cycles of the iBR combination followed by ibrutinib alone until progression. The ORR was 94%, with a 76% CR rate in patients with MCL. The recommended phase II dosage of ibrutinib was 560 mg/d in combination with BR. An ongoing randomized, double-blind, placebo-controlled phase III global study is comparing iBR with BR in patients with newly diagnosed MCL (the SHINE study, NCT01776840).
TO PUT THAT INTO CONTEXT
[[{"type":"media","view_mode":"media_crop","fid":"51922","attributes":{"alt":"","class":"media-image","id":"media_crop_1339700251112","media_crop_h":"0","media_crop_image_style":"-1","media_crop_instance":"6423","media_crop_rotate":"0","media_crop_scale_h":"0","media_crop_scale_w":"0","media_crop_w":"0","media_crop_x":"0","media_crop_y":"0","style":"height: 144px; width: 144px;","title":" ","typeof":"foaf:Image"}}]]
Anas Younes, MD
Memorial Sloan Kettering Cancer Center
New York, New YorkWhat New Agents Are Available for the Treatment of Lymphoid Malignancies?In the past 10 years, nearly a dozen drugs have been approved by the US Food and Drug Administration for the treatment of lymphoid malignancies; these agents include brentuximab vedotin, obinutuzumab, ibrutinib, idelalisib, lenalidomide, romidepsin, belinostat, pralatrexate, blinatumomab, and venetoclax. In May of this year, the immune checkpoint inhibitor nivolumab was approved for the treatment of relapsed Hodgkin lymphoma. The majority of agents fail due to unacceptable toxicity, low antitumor efficacy, and/or poor pharmacokinetic properties. Typically in lymphoma trials, agents that yield low response rates but have a good safety profile are combined with other agents in well-intentioned but unfocused clinical strategies; such combinations rarely succeed in obtaining regulatory approval.Today, the leading class of agents in development for the treatment of lymphoma are the B-cell receptor signaling inhibitors that target Bruton tyrosine kinase (BTK) and spleen tyrosine kinase, the phosphoinositide 3-kinase (PI3K) pathway inhibitors that target different PI3K isoforms, and the inhibitors of B-cell lymphoma-2 (BCL-2). Within each of these drug classes, the FDA has approved one agent. The BTK inhibitor ibrutinib is approved for the treatment of chronic lymphocytic leukemia (CLL), mantle cell lymphoma, and Waldenström macroglobulinemia; the PI3Kδ inhibitor idelalisib is approved for the treatment of CLL and follicular lymphoma; and the BCL-2 inhibitor venetoclax is approved for the treatment of CLL patients with 17p deletions. While it is clear that these drugs also have clinical activity in other lymphoma subsets, their efficacy in these groups is not sufficient to warrant FDA approval for use as single agents. Future research should focus on the identification of biomarkers that would enable patients to be selected for treatment with specific agents, and on the development of mechanism-based combination regimens. What Are Important Clinical Considerations for Use of New Therapies in Lymphoma?Because some of these new agents have unique mechanisms of action, unusual toxicities can arise that require special consideration. For example, first-generation BTK inhibitors are associated with atrial and bleeding disorders, idelalisib with gastrointestinal and infectious complications, and venetoclax with tumor lysis syndrome. Immune checkpoint inhibitors can cause immune-related toxicities that may affect the lungs, liver, skin, and kidneys.Thus, while the outlook for our patients with lymphoma seems promising, future oncologists and the healthcare team will require special training and skills to understand the molecular mechanisms underlying the use of these new agents, the genetic biomarkers that are identified through next-generation sequencing, and how best to identify and manage the unusual treatment-related toxicities.Financial Disclosure: Dr. Younes has received honoraria from Bayer, Bristol-Myers Squibb, Curis, Gilead, Incyte, Merck, Roche, and Takeda.
Ibrutinib in DLBCL and indolent NHL. The activated B-cell–like (ABC) subtype of DLBCL is characterized by chronic/constitutive BCR signaling and NF-kB activation, which can be targeted by ibrutinib.[15] In a phase I/II clinical trial with single-agent ibrutinib in patients with relapsed or refractory DLBCL, the ORR was 37% (14/38) in those with ABC DLBCL, compared with 5% (1/20) in those with germinal center B-cell–like (GCB) DLBCL.[16] Subsequent studies have evaluated ibrutinib combinations for DLBCL. Younes et al conducted a dose-escalation phase Ib study with iR-CHOP (ibrutinib plus R-CHOP [rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone]) in treatment-naive patients with DLBCL, MCL, and FL.[17] The recommended phase II dosage for ibrutinib was 560 mg daily. The most common grade ≥ 3 adverse events included neutropenia (73%), thrombocytopenia (21%), febrile neutropenia (18%), and anemia (18%). In patients with known DLBCL subtypes, 71% of the GCB DLBCL and 100% of the ABC DLBCL patients achieved a CR. Based on these encouraging signals in ABC DLBCL, a randomized phase III international study is ongoing that compares iR-CHOP with standard R-CHOP as first-line therapy in patients with ABC DLBCL (NCT01855750). In patients with relapsed DLBCL, ibrutinib is being evaluated in combination with chemoimmunotherapy (NCT02219737, NCT02142049) or with biologic combinations such as lenalidomide and rituximab (NCT02077166).
Single-agent ibrutinib has modest activity (30% ORR) in relapsed/refractory FL.[18] In the frontline setting, the doublet of ibrutinib and rituximab in treatment-naive patients with FL produced an ORR of 82%, with CRs in 27%.[19] Patients who received the triplet of ibrutinib, rituximab, and lenalidomide had an ORR of 91%, with CRs in 63%, comparable to results seen with the R2 (rituximab, lenalidomide) regimen, albeit with a significant incidence of rash (73% total, 32% grade 3).[20]
Emergence of resistance mechanisms. Primary and secondary mechanisms of resistance to ibrutinib have begun to be elucidated in lymphoma subtypes. In CLL, whole-exome deep sequencing identified a cysteine-to-serine mutation (C481S) in BTK at the binding site of ibrutinib in 5 of 6 patients who acquired resistance to ibrutinib. Additional gain-of-function mutations in PLCγ2-R665W and L845F-were identified in two patients, which allowed BCR signaling independent of BTK inhibition.[21] Although acquired resistance to ibrutinib remains infrequent, these data suggest that patients with high-risk CLL who have 17p13.1 deletion, 11q22.3 deletion, or a complex karyotype may be at increased risk for resistance because of genomic instability. Therefore, rational combination therapies may overcome or limit this resistance.[22] MCL expresses primary ibrutinib resistance by activation of distal BCR signaling via PI3K/AKT and NF-kB pathways. In DLBCL and WM, CXCR4, CARD11, and CD79A/B mutations also predict likelihood of response.[23] Understanding these mechanisms of resistance is important because resistance to ibrutinib prognosticates poor response to subsequent therapies, particularly in patients with MCL.[24,25]
Class-specific adverse events. Generally well tolerated, ibrutinib has a predictable and manageable toxicity profile, some of which may reflect its off-target inhibition of a number of kinases with a cognate cysteine, such as epidermal growth factor receptor (EGFR), TEC, and interleukin-2–inducible T-cell kinase (ITK).
• Bleeding/bruising: Bleeding-related episodes were increased with ibrutinib use. Although most were clinically insignificant, major hemorrhage was reportedly more frequent with ibrutinib (4%) than with chlorambucil (2%) in the RESONATE-2 study. In vitro studies pointed to ibrutinib inhibition of collagen-induced platelet aggregation and adhesion to von Willebrand factor,[26] and light transmission aggregometry detected decreased platelet aggregation in patients with bleeding complications.[27] This is in part caused by inhibition of integrin αIIbβ3 signaling, which leads to the formation of unstable thrombi.[28] Ibrutinib should be temporarily discontinued before invasive procedures and surgery.
• Atrial fibrillation: Atrial fibrillation has been reported in 3% to 6% of patients who receive ibrutinib and is typically managed medically with standard treatments, without changes in the dose of ibrutinib. The development of atrial fibrillation is thought to be related to the presence of BTK and TEC expressed in human heart tissue; both are targeted by ibrutinib. McMullen et al showed that ibrutinib decreases expression of the cardioprotective PI3K-AKT pathway, which leads to an increased susceptibility to atrial fibrillation.[29]
• Rash and diarrhea: The incidence of grade 1/2 rash and the incidence of diarrhea were increased among patients who received ibrutinib in phase III studies; grade ≥ 3 diarrhea occurred in up to 4%. Both adverse events were hypothesized to be related in part to the off-target inhibition of EGFR and ERBB2. In a single-institution study, additional skin and nail changes-including onychorrhexis, onychoschizia, and brittle toenails-which negatively affected quality of life, were reported in up to 67% of patients with CLL who were receiving long-term ibrutinib therapy.[30]
Second-generation BTK inhibitors
Compared with ibrutinib, acalabrutinib-a second-generation BTK inhibitor-has less off-target inhibition; an absence of irreversible inhibition of EGFR, TEC, and ITK without plasma accumulation; and a shorter half-life, which allows twice-daily dosing. Byrd et al performed a dose-escalation phase I study with a phase II fixed-dose expansion cohort in 61 patients with relapsed CLL.[31] At a median follow-up of 14.3 months, the ORR was 95%; all responses were PRs or PRs with lymphocytosis. An additional 5% of patients had stable disease. Of 18 patients who had 17p13.1 deletion, 100% responded. The one patient with progression had both BTK C481S and PLCγ2 L845F mutations, which implicates susceptibility to the same mechanisms of acquired resistance as are seen with ibrutinib. Safety results thus far have been favorable, and adverse events consist mostly of grade 1/2 headache, diarrhea, increased weight, pyrexia, and infections, without report of major hemorrhage or atrial fibrillation. In addition to examining the efficacy and safety of acalabrutinib in patients with CLL who are intolerant of ibrutinib therapy (NCT02717611), ongoing phase III studies are comparing acalabrutinib with ibrutinib in patients with relapsed high-risk CLL (NCT02477696) and are also comparing acalabrutinib monotherapy with either the combination of acalabrutinib plus obinutuzumab or the combination of chlorambucil plus obinutuzumab (NCT02475681).
PI3K Inhibitors
Mechanism of action
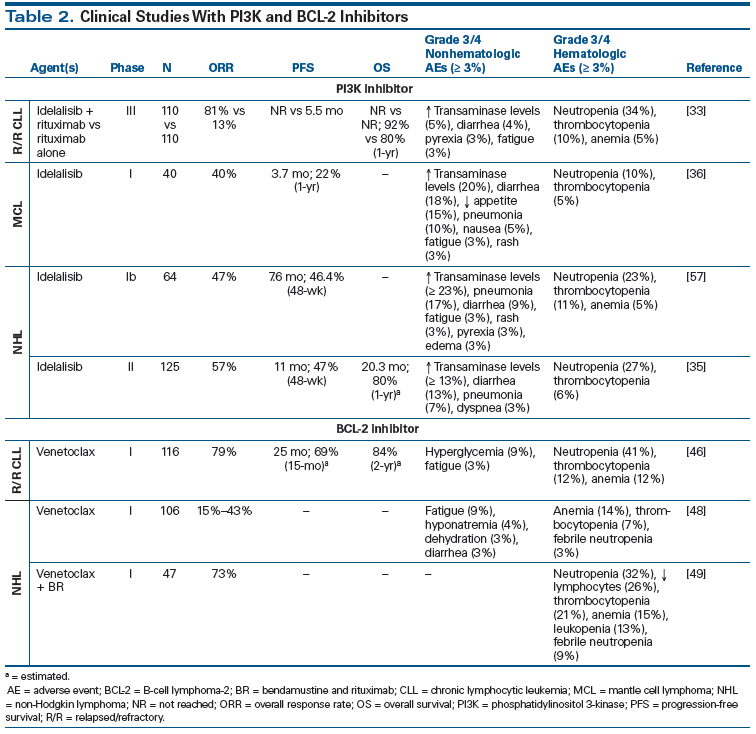
The BCR pathway involves signaling through PI3K, which activates downstream serine/threonine kinase AKT and mammalian target of rapamycin (mTOR) to promote proliferation, survival, motility, and angiogenesis. Class I PI3K has a catalytic subunit with four different isoforms-p110α, p110β, p110γ, and p110δ-with the delta isoform highly expressed in tissues of hematopoietic origin. Idelalisib is a potent, orally bioavailable PI3K inhibitor that is highly specific for the delta isoform, and it is the first drug of this class to be approved by the FDA for the treatment of CLL and FL. Other PI3K inhibitors in development include duvelisib (IPI-145), which inhibits both the PI3K delta and gamma isoforms, and copanlisib, which is a combined PI3K alpha/delta inhibitor (Table 2).
Clinical applications of idelalisib
Idelalisib in CLL. Based on encouraging phase I/II results of the efficacy of single-agent idelalisib in relapsed or refractory CLL,[32] Furman et al conducted a global phase III randomized trial of combination idelalisib and rituximab in 220 patients with relapsed CLL to assess PFS.[33] More than 40% of patients had a 17p deletion or TP53 mutation, and more than 80% had unmutated IGHV. Patients were randomly assigned to idelalisib at a dosage of 150 mg orally twice daily or placebo.
The study was terminated early because of the significant efficacy of idelalisib at interim analysis. The PFS was 93% at 24 weeks in the idelalisib group vs 46% in the placebo group, and the improved PFS with idelalisib was seen across all risk subgroups. The OS in the idelalisib group at 1 year was 92%, compared with 80% in the placebo group. The ORR was 81% with idelalisib vs 13% with placebo. The addition of rituximab to idelalisib blunted and shortened the duration of lymphocytosis. The most common adverse events with idelalisib were pyrexia, fatigue, nausea, chills, and diarrhea, and idelalisib was associated with increased gastrointestinal and skin complications. Grade ≥ 3 diarrhea was reported in four patients, rash in two, and elevated transaminase levels in six, which were not seen in the placebo group. These results led to the FDA approval of idelalisib for relapsed or refractory CLL in combination with rituximab in 2014, although a boxed warning was mandated for hepatotoxicity, severe diarrhea or colitis, pneumonitis, and intestinal perforation.
The idelalisib plus rituximab combination was also evaluated as first-line therapy in 64 patients with CLL/SLL by O’Brien et al.[34] The ORR was 97%, including 19% with CRs. The ORR was 100% in patients with 17p deletion/TP53 mutations and 97% in those with unmutated IGHV. PFS was 83% at 36 months.
Idelalisib in NHL. Gopal et al evaluated single-agent idelalisib, given at a dosage of 150 mg twice daily continuously, in 125 patients with indolent NHLs refractory to both rituximab and an alkylating drug.[35] The ORR was 57%, ranging from 47% to 80% across subgroups, including 54% in FL and 61% in SLL. The median time to response was 1.9 months; the median duration of response, 12.5 months; the median PFS, 11 months; and OS, 20.3 months. The most common grade ≥ 3 adverse events were neutropenia (27%), diarrhea (13%), elevated transaminase levels (13%), pneumonia (7%), and dyspnea (3%). Grade ≥ 3 colitis, diarrhea, or both were reported in 20 patients (16%) at a median of 6 months after treatment initiation. The FDA granted idelalisib accelerated approval in 2014 for patients with FL and SLL who have received at least two prior systemic therapies.
Single-agent idelalisib has also shown clinical activity in patients with MCL in a phase I dose escalation and extension trial.[36] The ORR was 40%, with CRs in 5% and PRs in 35%. Patients who received ≥ 150 mg twice daily had an ORR of 69%. The median time to response was 1.1 months, and the median duration of response was 2.7 months. These data provide proof of concept that targeting PI3Kδ is a viable strategy in MCL.
Idelalisib-associated adverse events. A number of complications that were evident from the clinical trials with idelalisib resulted in black box warnings for severe and/or fatal diarrhea or colitis, hepatotoxicity, pneumonitis, and intestinal perforation. Additional warnings include severe cutaneous reactions, anaphylaxis, neutropenia, and embryo-fetal toxicity. Anaphylaxis and grade ≥ 3 cutaneous reactions, including toxic epidermal necrolysis, should prompt immediate discontinuation of the drug. Grade 3/4 neutropenia may be managed with dose modification ± granulocyte colony-stimulating factor. Elevation of aspartate aminotransferase (AST) or alanine aminotransferase (ALT) levels to > 5 times the upper limit of normal usually occurred within the first 12 weeks of treatment and typically resolved with a temporary drug hold and dose reduction. The pneumonitis is thought to derive from a hypersensitivity reaction that has also been observed with mTOR inhibitors.[37]
Diarrhea and colitis were the most common adverse events (any grade, up to 21%–47%; grade ≥ 3, 5%–14%), leading to discontinuation of idelalisib across trials. The colitis and diarrhea were treated with either a temporary drug hold, with or without dose reduction, or termination of the study involvement. The diarrhea presented as one of two types: either a self-limiting form responsive to antidiarrheal agents that occurs within 8 weeks of treatment, or a later-onset (> 8 weeks), more severe form that sometimes requires empiric budesonide or systemic corticosteroids.[37] The cause of the diarrhea and colitis is not clearly understood, but histopathology suggests drug-mediated immune dysregulation that causes mucosal injury. Findings are consistent with a characteristic triad of intraepithelial lymphocytosis, epithelial cell apoptosis, and neutrophilic cryptitis similar to that seen in mouse models with mutant PI3Kδ and an associated inflammatory bowel disease.[38]
Novel combinations with idelalisib may lead to unexpected serious toxicities and therefore warrant vigilance. In March 2016, six frontline phase III studies with idelalisib-containing combinations were stopped because of an increased risk of adverse events that were mostly infectious but included an increased risk of death. Previous phase I trials with idelalisib in combination with lenalidomide and rituximab were stopped early because of unexpected cytokine release syndrome and serious hepatotoxicity in patients with relapsed/refractory indolent NHL.[39]
Next-generation PI3K inhibitors
Dreyling et al conducted a phase IIa trial with single-agent copanlisib, a pan-PI3K inhibitor with potent PI3Kδ and PI3Kα inhibition.[40] In 33 patients with indolent NHL, the ORR was 47% for all patients. Grade 3/4 adverse events included hypertension, neutropenia, hyperglycemia, and anemia. Duvelisib is a novel targeted oral PI3Kδ and PI3Kγ inhibitor that has shown activity in patients with relapsed/refractory B-cell NHL and T-cell lymphoma in phase I trials, with ORRs of 65% and 42%, respectively. The most common grade ≥ 3 adverse events (all causality, ≥ 15%) were increased ALT/AST levels, diarrhea, and transient neutropenia.[41,42] TGR-1202 is a next-generation oral PI3Kδ inhibitor that has activities in relapsed/refractory CLL and NHL and notably lacks hepatotoxicity. When combined with ublituximab, a glycoengineered chimeric monoclonal antibody against CD20, an ORR of 57% was achieved across all subtypes, with an ORR of 80% in five patients with CLL.[43] Other novel PI3K inhibitor combination therapies show potential promise, such as the dual histone deacetylase (HDAC) and PI3K inhibitor CUDC-907, which demonstrated an ORR of 55% in patients with relapsed/refractory DLBCL.[44]
BCL-2 Inhibitors
Mechanism of action
BCL-2 family proteins are key regulators of apoptosis. Pharmacologic inhibition of prosurvival protein represents a promising therapeutic strategy for BCL-2–dependent hematologic malignancies. BH3-mimetic drugs, which compete for the BCL-2 hydrophobic BH3 domain–binding cleft, displace the prodeath proteins to allow their interaction with BAX and BAK, thereby triggering apoptosis. The first-generation BH3-mimetic drug navitoclax (ABT-263) showed clinical activity but had the dose-limiting toxicity of thrombocytopenia caused by concomitant on-target inhibition of BCL-XL in platelets. The second-generation BCL-2 inhibitor venetoclax (ABT-199), an orally bioavailable BCL-2 selective inhibitor that spares platelets, is in active clinical development in CLL and NHL subtypes (see Table 2).[45]
Clinical applications of venetoclax
Venetoclax in CLL. The first-in-human, phase I dose escalation and expansion trial was conducted in 116 patients with relapsed or refractory CLL or SLL to assess safety and efficacy.[46] The median number of prior therapies was three, and 89% of patients had adverse prognostic features, including resistance to fludarabine, 17p deletion, 11q deletion, unmutated IGHV, and bulky adenopathy. Tumor lysis syndrome occurred in 3 of 56 patients in the dose-escalation cohort. This led to a ramp-up design that required inpatient admissions and prophylaxis for tumor lysis syndrome before the first ramp-up dose of 50 mg for all patients, as well as hospitalizations for each ramp-up in high-risk patients. In total, tumor lysis syndrome occurred in 10 of 56 patients (18%). The most common grade 1/2 adverse events were diarrhea, nausea, and upper respiratory tract infections. The most common grade 3/4 adverse event was neutropenia (41%), which was responsive to growth factor therapy. A maximum tolerated dose was not identified, and patients received up to 400 mg of venetoclax daily in the dose-expansion cohort. For all 116 patients, the ORR was 79%, with a 20% CR rate, including 5% who achieved minimal residual disease as measured by flow cytometry. The 15-month PFS was 66%, and the estimated 2-year OS for all patients was 84%. Progression of disease occurred in 41 patients (35%) and was more common in those with 17p deletion.
The pivotal international phase II trial in ultra-high-risk patients secured FDA approval for venetoclax in CLL patients with 17p deletion who had at least one prior therapy.[47] The study enrolled 107 patients with relapsed/refractory 17p deletion CLL, assessed in the peripheral blood by a central laboratory with a Vysis fluorescence in situ hybridization probe. The participants received venetoclax once daily, with a weekly dose ramp-up schedule (20, 50, 100, 200, 400 mg) over a period of 5 weeks along with tumor lysis syndrome prophylaxis. Patients were treated with daily 400-mg continuous dosing until disease progression or unacceptable toxicity occurred. The ORR was 79.4%; the median time to first response was 0.8 months, with a median time to CR of 8.2 months. The estimated 12-month PFS was 72% and OS, 86.7%. In 18 of 45 patients who had an assessment for minimal residual disease, the results were negative. The most common adverse events were neutropenia (43%), diarrhea (29%), nausea (29%), anemia (27%), and fatigue (22%). Grade ≥ 3 adverse events were hematologic: neutropenia (40%), anemia (18%), and thrombocytopenia (11%). Laboratory tumor lysis syndrome occurred in 5 patients, none of whom had clinical sequelae.
Ongoing studies with venetoclax in combinations include doublets of venetoclax plus rituximab in relapsed/refractory CLL (NCT01682616), venetoclax plus obinutuzumab (NCT01685892), and a triplet of venetoclax plus ibrutinib and obinutuzumab (NCT02427451), with the goal of improving the CR rate and reducing minimal residual disease.
Venetoclax in NHL. Venetoclax has been evaluated as a single agent and in combination therapy in patients with B-cell NHL. A phase I dose-escalation trial of venetoclax monotherapy began with a 3-week ramp-up schedule starting at 200 mg in the dose-escalation cohort and 400 mg in the safety-expansion cohort. There were no reports of tumor lysis syndrome.[48] The ORR was 15% in patients with DLBCL, 43% in those with Richter’s transformation, and 34% in those with FL. The median duration of response was 10 months (range, 1–30 months).
In an ongoing phase I dose-escalation study, venetoclax has been combined with BR for patients with relapsed/refractory NHL (NCT01594229).[49] Patients were treated with oral venetoclax (50–800 mg) for 3, 7, or 28 consecutive days of each 28-day cycle, while the BR regimen was administered for 6 cycles. The study has so far enrolled 47 patients: 27 with FL, 15 with DLBCL, and 5 with marginal zone lymphoma (MZL). The most common adverse events were nausea (51%), thrombocytopenia (45%), neutropenia (40%), constipation (36%), anemia (34%), diarrhea (30%), fatigue (30%), and hyperglycemia (30%). Grade 3/4 adverse events were caused by neutropenia (32%), thrombocytopenia (21%), and anemia (15%). Of 38 evaluable patients, 29 (73%) responded. Other ongoing combination studies include a venetoclax-plus-ibrutinib doublet in MCL (NCT02419560) and venetoclax, ibrutinib, and obinutuzumab triplet in MCL (NCT02558816).
Other Novel Small-Molecule Inhibitors
Selective inhibitor of nuclear export
Selinexor is a selective inhibitor of nuclear export-a first-in-class, oral, covalent inhibitor of XPO1, a nuclear export protein. XPO1 is a karyopherin that mediates the nuclear export of more than 200 cellular regulatory proteins, including tumor suppressors. Most types of cancer overexpress XPO1, with increased nuclear export of tumor suppressors. Selinexor induces apoptosis of malignant cells by nuclear retention and activation of tumor suppressor proteins, as well as by inhibition of nuclear transport and translation of oncogenic messenger RNA (mRNA).
In a phase I study with 58 patients, selinexor was evaluated as a single agent in relapsed/refractory NHL and aggressive NHL across 13 dose levels, ranging from 3 to 80 mg/m2.[50] XPO1 mRNA levels were increased at all doses and sustained for 4 to 48 hours, which supports twice-weekly dosing. The recommended phase II dose is 60 mg/m2. The most common grade 1/2 adverse events were nausea (66%), anorexia (47%), fatigue (40%), and vomiting (40%). Grade 3/4 events included thrombocytopenia (31%), neutropenia (22%), fatigue (10%), and anemia (7%). The ORRs observed across all NHL subtypes included 40% at a dose of 60 mg/m2, 33% at 23–50 mg/m2, and 25% at 20 mg/m2.
A dose-finding study used a flat dose of 45–160 mg administered twice weekly in heavily pretreated patients with myeloma, NHL, and acute myeloid leukemia.[51] The ORR was comparable in the 45–65-mg and >65-mg dose groups (23% and 24%, respectively), although the >65-mg dose group had higher-grade adverse events. The rate of grade 3/4 thrombocytopenia was similar in both groups: 32% vs 39%. Based on these findings, a flat dose of 60 mg of selinexor, administered twice weekly, is the recommended phase II dose for patients with hematologic cancers. Additional studies are evaluating selinexor in combination with chemotherapy (eg, with rituximab, ifosfamide, carboplatin, and etoposide [RICE]; NCT02471911) or biologic agents (eg, with ibrutinib; NCT02303392).
Epigenetic inhibitors
Enhancer of zeste homolog 2 (EZH2) inhibitors. EZH2, a histone-lysine N-methyltransferase enzyme, is the catalytic subunit of polycomb repressor complex 2 (PRC2), which catalyzes the methylation of lysine 27 of histone H3. PRC2 represses gene expression and regulates cell proliferation and differentiation. EZH2 mutations, which have been identified in several germinal center subtypes of NHL-including GCB-type DLBCL, FL, and primary mediastinal large B-cell lymphoma-lead to hypertrimethylation of histone H3, which induces oncogenesis. Small inhibitors of EZH2 are currently being studied in phase I trials.
Tazemetostat (EPZ-6438) is an oral, selective inhibitor of EZH2. In the first-in-human study of tazemetostat in patients with NHL and solid tumors, the drug was administered orally twice daily in five dose cohorts and one food-effect cohort.[52] Of the 15 evaluable patients with NHL, responses were seen in 5 of 9 patients with DLBCL, 3 of 5 with FL, and 1 with MZL. The majority of objective responses occurred at the recommended phase II dose of 800 mg twice daily, and the drug was active in DLBCL regardless of EZH2 mutation or subtype. Adverse events that occurred in > 10% of patients were asthenia, anorexia, constipation, nausea, dysgeusia, vomiting, and muscle spasms. Grade ≥ 3 adverse events included thrombocytopenia, neutropenia, hypertension, anorexia, and elevated transaminase levels. Targeting epigenetic modifiers is an area of growing research interest, with emerging data that will likely be incorporated into larger clinical trials.
HDAC inhibitors. By blocking HDAC enzymes, HDAC inhibitors can hyperacetylate histones in cells and cause transcriptional activation of tumor suppressor genes, as well as genes involved in proliferation and apoptosis, resulting in antitumor activity. Abexinostat, an orally available hydroxamate-containing HDAC inhibitor, allows for continuous exposure with manageable toxicity. Abexinostat was recently shown to have an ORR of 56%, 40%, and 31% in FL, T-cell lymphoma, and DLBCL, respectively.[53]
Other HDAC inhibitors have also shown promising responses as monotherapy or in combinations. The pan-HDAC inhibitor belinostat was shown to be safe and effective in combination with CHOP chemotherapy in patients with peripheral T-cell lymphoma; the ORR was 89%, with CRs in 72%.[54] Synergistic antitumor effects achieved with HDAC inhibitor and PI3K inhibitor combinations in various DLBCL xenograft models have provided a strong rationale for testing a highly potent dual HDAC and PI3K inhibitor, CUDC-907. Preliminary results from a phase I study showed a 55% ORR in 11 patients with DLBCL; dose expansion and phase II studies are now enrolling.[44]
Conclusions
Small-molecule inhibitors are changing the way we manage B-cell lymphoma and CLL, making effective treatment in the form of long-term therapy with oral agents a reality for many patients. This has affected how we select patients for treatment, when we start therapy, how we assess response, and what we can expect in terms of treatment-emergent side effects.
CLL appears highly responsive to biologic agents that target signaling transduction downstream of BCRs: namely, BTK inhibitors and PI3K inhibitors, as well as BCL-2 inhibitors. When selecting treatment, physicians should take into consideration clinical indications, interaction of coexisting medical conditions with potential side-effect profiles of different agents, and patient preferences. The efficacy of ibrutinib and idelalisib also arises from disruption of the localization of malignant B cells in their protective niches in lymph nodes, releasing tumor cells into the bloodstream, with transient relocation lymphocytosis observed in most CLL patients treated with these agents. To avoid premature cessation of effective treatment, response criteria and guidelines for CLL have been modified and now include a category of “PR with lymphocytosis.”[55]
It is noteworthy that single-agent ibrutinib and idelalisib do not produce durable responses in all patients and rarely produce complete remissions. Identifying and overcoming resistance mechanisms will be crucial for the most effective use of these agents, especially in high-risk patients. Combination strategies, involving either other novel agents or chemoimmunotherapy, are in active clinical development in both the relapsed and frontline settings, with the goal of improving the CR rate and achieving minimal residual disease to extend survival. One appealing agent is the BCL-2 inhibitor venetoclax, which is capable of inducing a CR and minimal residual disease in CLL patients with 17p deletion.
In aggressive NHL, small-molecule inhibitors continue to carve out emerging therapeutic niches, both as single-agent therapy and in combination regimens in selected subtypes. In MCL, single-agent ibrutinib has demonstrated efficacy in relapsed disease, while studies of ibrutinib in combination with BR chemoimmunotherapy are ongoing in the first-line setting. Increased levels of PI3K/AKT/mTOR/MCL-1 in ibrutinib-resistant MCL cell lines have provided a rationale for designing salvage treatment with a PI3K inhibitor (NCT02455297) for ibrutinib-resistant disease.[56] In DLBCL, selective targeting of the BCR signaling pathway by ibrutinib has proved to be effective in the non-GCB subtype. This concept is being tested in an ongoing phase III study that incorporates ibrutinib into frontline R-CHOP for patients with non-GCB DLBCL (NCT01855750). An additional strategy for non-GCB DLBCL involves targeting parallel pathogenic pathways, such as combining ibrutinib and lenalidomide to synergistically inhibit NF-kB and trigger apoptosis. Selective inhibitors of nuclear export and epigenetic modifier EZH2 have also demonstrated promising clinical signals. It is hoped that emerging molecular mechanisms and bioinformatics knowledge will continue to tailor targeted therapy for optimal clinical benefit, while minimizing the development of treatment resistance.
Financial Disclosure:Dr. Ruan receives research funding from Celgene, Janssen, Pharmacyclics, and Seattle Genetics; and has served as a consultant, speaker, or advisory board member for Celgene, Janssen, Pharmacyclics, and Seattle Genetics. Dr. Choe has no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
References:
1. Rickert RC. New insights into pre-BCR and BCR signalling with relevance to B cell malignancies. Nat Rev Immunol. 2013;13:578-91.
2. ten Hacken E, Burger JA. Molecular pathways: targeting the microenvironment in chronic lymphocytic leukemia-focus on the B-cell receptor. Clin Cancer Res. 2014;20:548-56.
3. Byrd JC, Furman RR, Coutre SE, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med. 2013;369:32-42.
4. Byrd JC, Brown JR, O’Brien S, et al. Ibrutinib versus ofatumumab in previously treated chronic lymphoid leukemia. N Engl J Med. 2014;371:213-23.
5. Burger JA, Tedeschi A, Barr PM, et al. Ibrutinib as initial therapy for patients with chronic lymphocytic leukemia. N Engl J Med. 2015;373:2425-37.
6. Burger JA, Keating MJ, Wierda WG, et al. Safety and activity of ibrutinib plus rituximab for patients with high-risk chronic lymphocytic leukaemia: a single-arm, phase 2 study. Lancet Oncol. 2014;15:1090-9.
7. Chanan-Khan A, Cramer P, Demirkan F, et al. Ibrutinib combined with bendamustine and rituximab compared with placebo, bendamustine, and rituximab for previously treated chronic lymphocytic leukaemia or small lymphocytic lymphoma (HELIOS): a randomised, double-blind, phase 3 study. Lancet Oncol. 2016;17:200-11.
8. Treon SP, Xu L, Hunter Z. MYD88 mutations and response to ibrutinib in Waldenström’s macroglobulinemia. N Engl J Med. 2015;373:584-6.
9. Treon SP, Tripsas CK, Meid K, et al. Ibrutinib in previously treated Waldenström’s macroglobulinemia. N Engl J Med. 2015;372:1430-40.
10. Wang ML, Rule S, Martin P, et al. Targeting BTK with ibrutinib in relapsed or refractory mantle-cell lymphoma. N Engl J Med. 2013;369:507-16.
11. Wang ML, Blum KA, Martin P, et al. Long-term follow-up of MCL patients treated with single-agent ibrutinib: updated safety and efficacy results. Blood. 2015;126:739-45.
12. Dreyling M, Jurczak W, Jerkeman M, et al. Ibrutinib versus temsirolimus in patients with relapsed or refractory mantle-cell lymphoma: an international, randomised, open-label, phase 3 study. Lancet. 2016;387:770-8.
13. Wang ML, Lee H, Chuang H, et al. Ibrutinib in combination with rituximab in relapsed or refractory mantle cell lymphoma: a single-centre, open-label, phase 2 trial. Lancet Oncol. 2016;17:48-56.
14. Maddocks K, Christian B, Jaglowski S, et al. A phase 1/1b study of rituximab, bendamustine, and ibrutinib in patients with untreated and relapsed/refractory non-Hodgkin lymphoma. Blood. 2015;125:242-8.
15. Davis RE, Ngo VN, Lenz G, et al. Chronic active B-cell-receptor signalling in diffuse large B-cell lymphoma. Nature. 2010;463:88-92.
16. Wilson WH, Young RM, Schmitz R, et al. Targeting B cell receptor signaling with ibrutinib in diffuse large B cell lymphoma. Nat Med. 2015;21:922-6.
17. Younes A, Thieblemont C, Morschhauser F, et al. Combination of ibrutinib with rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone (R-CHOP) for treatment-naive patients with CD20-positive B-cell non-Hodgkin lymphoma: a non-randomised, phase 1b study. Lancet Oncol. 2014;15:1019-26.
18. Bartlett NL, LaPlant BR, Qi J, et al. Ibrutinib monotherapy in relapsed/refractory follicular lymphoma (FL): preliminary results of a phase 2 consortium (P2C) trial. Blood. 2014;124(suppl 21):abstr 800.
19. Fowler N, Nastoupil L, de Vos S, et al. Ibrutinib plus rituximab in treatment-naive patients with follicular lymphoma: results from a multicenter, phase 2 study. Blood. 2015;126(suppl 23):abstr 470.
20. Ujjani CS, Jung S-H, Pitcher B, et al. Phase I study of rituximab, lenalidomide, and ibrutinib in previously untreated follicular lymphoma (Alliance 051103). Blood. 2015;126(suppl 23):abstr 471.
21. Woyach JA, Furman RR, Liu T-M, et al. Resistance mechanisms for the Bruton’s tyrosine kinase inhibitor ibrutinib. N Engl J Med. 2014;370:2286-94.
22. Cheng S, Guo A, Lu P, et al. Functional characterization of BTKC481S mutation that confers ibrutinib resistance: exploration of alternative kinase inhibitors. Leukemia. 2015;29:895-900.
23. Zhang SQ, Smith SM, Zhang SY, Lynn Wang Y. Mechanisms of ibrutinib resistance in chronic lymphocytic leukaemia and non-Hodgkin lymphoma. Br J Haematol. 2015;170:445-56.
24. Cheah CY, Chihara D, Romaguera JE, et al. Patients with mantle cell lymphoma failing ibrutinib are unlikely to respond to salvage chemotherapy and have poor outcomes. Ann Oncol. 2015;26:1175-9.
25. Martin P, Maddocks K, Leonard JP, et al. Postibrutinib outcomes in patients with mantle cell lymphoma. Blood. 2016;127:1559-63.
26. Levade M, David E, Garcia C, et al. Ibrutinib treatment affects collagen and von Willebrand factor-dependent platelet functions. Blood. 2014;124:3991-5.
27. Kamel S, Horton L, Ysebaert L, et al. Ibrutinib inhibits collagen-mediated but not ADP-mediated platelet aggregation. Leukemia. 2015;29:783-7.
28. Bye AP, Unsworth AJ, Vaiyapuri S, et al. Ibrutinib inhibits platelet integrin αIIb β3 outside-in signaling and thrombus stability but not adhesion to collagen significance. Arterioscler Thromb Vasc Biol. 2015;35:2326-35.
29. McMullen JR, Boey EJ, Ooi JY, et al. Ibrutinib increases the risk of atrial fibrillation, potentially through inhibition of cardiac PI3K-Akt signaling. Blood. 2014;124:3829-30.
30. Bitar C, Farooqui MZ, Valdez J, et al. Hair and nail changes during long-term therapy with ibrutinib for chronic lymphocytic leukemia. JAMA Dermatol. 2016;152:698-701.
31. Byrd JC, Harrington B, O’Brien S, et al. Acalabrutinib (ACP-196) in relapsed chronic lymphocytic leukemia. N Engl J Med. 2016;374:323-32.
32. Brown JR, Byrd JC, Coutre SE, et al. Idelalisib, an inhibitor of phosphatidylinositol 3-kinase p110δ, for relapsed/refractory chronic lymphocytic leukemia. Blood. 2014;123:3390-7.
33. Furman RR, Sharman JP, Coutre SE, et al. Idelalisib and rituximab in relapsed chronic lymphocytic leukemia. N Engl J Med. 2014;370:997-1007.
34. O’Brien SM, Lamanna N, Kipps TJ, et al. A phase 2 study of idelalisib plus rituximab in treatment-naïve older patients with chronic lymphocytic leukemia. Blood. 2015;126:2686-94.
35. Gopal AK, Kahl BS, de Vos S, et al. PI3Kδ inhibition by idelalisib in patients with relapsed indolent lymphoma. N Engl J Med. 2014;370:1008-18.
36. Kahl BS, Spurgeon SE, Furman RR, et al. A phase 1 study of the PI3Kδ inhibitor idelalisib in patients with relapsed/refractory mantle cell lymphoma (MCL). Blood. 2014;123:3398-405.
37. Coutre SE, Barrientos JC, Brown JR, et al. Management of adverse events associated with idelalisib treatment: expert panel opinion. Leuk Lymphoma. 2015;56:2779-86.
38. Weidner A-S, Panarelli NC, Geyer JT, et al. Idelalisib-associated colitis: histologic findings in 14 patients. Am J Surg Pathol. 2015;39:1661-7.
39. Cheah CY, Nastoupil LJ, Neelapu SS, et al. Lenalidomide, idelalisib, and rituximab are unacceptably toxic in patients with relapsed/refractory indolent lymphoma. Blood. 2015;125:3357-9.
40. Dreyling M, Cunningham D, Bouabdallah K, et al. Phase 2A study of copanlisib, a novel PI3K inhibitor, in patients with indolent lymphoma. Blood. 2014;124(suppl 21):abstr 1701.
41. Flinn I, Oki Y, Patel M, et al. A phase 1 evaluation of duvelisib (IPI-145), a PI3K-δ,γ inhibitor, in patients with relapsed/refractory iNHL. Blood. 2014;124(suppl 21):abstr 802.
42. Horwitz SM, Porcu P, Flinn I, et al. Duvelisib (IPI-145), a phosphoinositide-3-kinase-δ,γ inhibitor, shows activity in patients with relapsed/refractory T-cell lymphoma. Blood. 2014;124(suppl 21):abstr 803.
43. Lunning MA, Vose JM, Schreeder MT, et al. Ublituximab, a novel glycoengineered anti-CD20 monoclonal antibody (mAb), in combination with TGR-1202, a next generation once daily PI3kδ inhibitor, demonstrates activity in heavily pre-treated and high-risk chronic lymphocytic leukemia (CLL) and B-cell lymphoma. Blood. 2014;124(suppl 21):abstr 801.
44. Younes A, Berdeja J, Patel MR, et al. Phase 1 trial testing single agent CUDC-907, a novel, oral dual inhibitor of histone deacetylase (HDAC) and PI3K: initial assessment of patients with relapsed or refractory (RR) diffuse large B-cell lymphoma (DLBCL), including double expressor (DE) lymphoma. Blood. 2015;126(suppl 23):abstr 257.
45. Souers AJ, Leverson JD, Boghaert ER, et al. ABT-199, a potent and selective BCL-2 inhibitor, achieves antitumor activity while sparing platelets. Nat Med. 2013;19:202-8.
46. Roberts AW, Davids MS, Pagel JM, et al. Targeting BCL2 with venetoclax in relapsed chronic lymphocytic leukemia. N Engl J Med. 2016;374:311-22.
47. Stilgenbauer S, Eichhorst B, Schetelig J, et al. Venetoclax (ABT-199/GDC-0199) monotherapy induces deep remission, including complete remission and undetectable MRD, in ultra-high risk relapsed/refractory chronic lymphocytic leukemia with 17p deletion: results of the pivotal international phase 2 study. Blood. 2015;126(suppl 23):abstr LBA-6.
48. Gerecitano JF, Roberts AW, Seymour JF, et al. A phase 1 study of venetoclax (ABT-199/GDC-0199) monotherapy in patients with relapsed/refractory non-Hodgkin lymphoma. Blood. 2015;126(suppl 23):abstr 254.
49. de Vos S, Swinnen L, Kozloff M, et al. A dose-escalation study of venetoclax (ABT-199/GDC-0199) in combination with bendamustine and rituximab in patients with relapsed or refractory non-Hodgkin’s lymphoma. Blood. 2015;126(suppl 23):abstr 255.
50. Kuruvilla J, Byrd JC, Flynn JM, et al. The oral selective inhibitor of nuclear export (SINE) selinexor (KPT-330) demonstrates broad and durable clinical activity in relapsed/refractory non Hodgkin’s lymphoma (NHL). Blood. 2014;124(suppl 21):abstr 396.
51. Chen C, Garzon R, Gutierrez M, et al. Safety, efficacy, and determination of the recommended phase 2 dose for the oral selective inhibitor of nuclear export (SINE) selinexor (KPT-330). Blood. 2015;126(suppl 23):abstr 258.
52. Ribrag V, Soria J-C, Michot J-M, et al. Phase 1 study of tazemetostat (EPZ-6438), an inhibitor of enhancer of zeste-homolog 2 (EZH2): preliminary safety and activity in relapsed or refractory non-Hodgkin lymphoma (NHL) patients. Blood. 2015;126(suppl 23):abstr 473.
53. Ribrag V, Kim WS, Bouabdallah R, et al. Safety and efficacy of abexinostat, a pan-histone deacetylase (HDAC) inhibitor, in non-Hodgkin lymphoma and chronic lymphocytic leukemia: results of an ongoing phase 2 study. Blood. 2015;126(suppl 23):abstr 256.
54. Johnston P, Cashen A, Nikolinakos P, et al. Safe and effective treatment of patients with peripheral T-cell lymphoma (PTCL) with the novel HDAC inhibitor, belinostat, in combination with CHOP: results of the Bel-CHOP phase 1 trial. Blood. 2015;126(suppl 23):abstr 253.
55. Cheson BD, Byrd JC, Rai KR, et al. Novel targeted agents and the need to refine clinical end points in chronic lymphocytic leukemia. J Clin Oncol. 2012;30:2820-2.
56. Pham L, Zhang L, Tao W, et al. Developing novel therapeutic strategies to overcome ibrutinib resistance in mantle cell lymphoma. Blood. 2015;126(suppl 23):abstr 707.
57. Flinn IW, Kahl BS, Leonard JP, et al. Idelalisib, a selective inhibitor of phosphatidylinositol 3-kinase-δ, as therapy for previously treated indolent non-Hodgkin lymphoma. Blood. 2014;123:3406-13.