Nilotinib Effective for Imatinib-Resistant CML
Nilotinib offers good results for patients with Philadelphia chromosome-positive chronic myeloid leukemia (CML) in chronic phase who are resistant or intolerant of imatinib, according to 48-month follow-up results of a phase II study.
Nilotinib offers good results for patients with Philadelphia chromosome-positive chronic myeloid leukemia (CML) in chronic phase who are resistant or intolerant of imatinib, according to 48-month follow-up results of a phase II study.
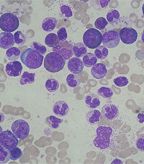
CML: marked leucocytosis with granulocyte left shift; source: Paulo Henrique Orlandi Mourao, Wikimedia Commons
Imatinib (Gleevec) is an effective treatment for CML, but not in all patients. “Approximately 25% to 30% of patients discontinue imatinib within 5 years because of unsatisfactory response, resistance or toxicity,” wrote researchers led by Frank Giles, director of HRB Clinical Research Facilities Galway in Ireland, online ahead of print in Leukemia.
Giles and colleagues reported on 48-month follow-up data for a multicenter phase II trial; at 24 months, nilotinib (Tasigna) 400 mg twice daily was effective in imatinib-resistant or imatinib-intolerant patients. The latest results include 321 patients, 226 of whom (70%) were imatinib resistant and 95 of whom (30%) were imatinib intolerant; patients received imatinib for a median of 32 months prior to entering the study.
After 48 months, 224 patients (70%) had discontinued the study; this was due to disease progression in 96 patients and adverse events in 66 patients. The progression-free survival rate at 48 months was 57%, and only 11 of 102 patients with PFS events progressed to accelerated phase or blast phase. Overall survival at 48 months was 78%, and the median survival time had not yet been reached.
Patients who had a complete hematologic response at baseline had a PFS of 71% compared to 49% for those who did not (P = 0.001). “This suggests that switching patients to nilotinib therapy before hematological failure on imatinib, in accordance with current treatment recommendations, may maximize the efficacy of nilotinib,” the investigators wrote.
A total of 190 patients (59%) achieved a major cytogenetic response at the 24-month update, and no additional patients achieved such a response between 24 and 48 months. Five patients did improve from a partial to a complete cytogenetic response since the 24-month analysis.
“Minimal new hematological toxicity was observed with nilotinib since the 24-month analysis,” the researchers wrote. New or worsening grade 3 or 4 neutropenia and thrombocytopenia occurred in only three patients between 24 and 48 months. Nonhematologic toxicities included rash and nausea, and no new grade 3 or 4 nonhematologic toxicities occurred since 24 months.
In an e-mail to CancerNetwork, Dr. Giles said the results are consistent with prior data on nilotinib and other second line tyrosine kinase inhibitors. He said that nilotinib is likely best used as a first line therapy, and a research priority now is the optimization of frontline nilotinib. The phase III ENEST1st trial is currently studying nilotinib as a first-line treatment for patients with Philadelphia chromosome-positive CML in chronic phase. Dr. Giles also said efforts should be made to find “novel agents for patients with a suboptimal response or failure.”