Nonadherence to Breast Cancer Screening Guidelines Prevalent in High-Risk Group
Patients at high risk for breast cancer appear to have higher rates of nonadherence to screening guidelines vs those at average risk.
"Our results are consistent with prior studies, which have found underutilization of supplemental screening modalities, particularly MRI, among [patients] who are at high risk for breast cancer, indicating potential underscreening for an at-risk population of [patients]," according to the study authors.
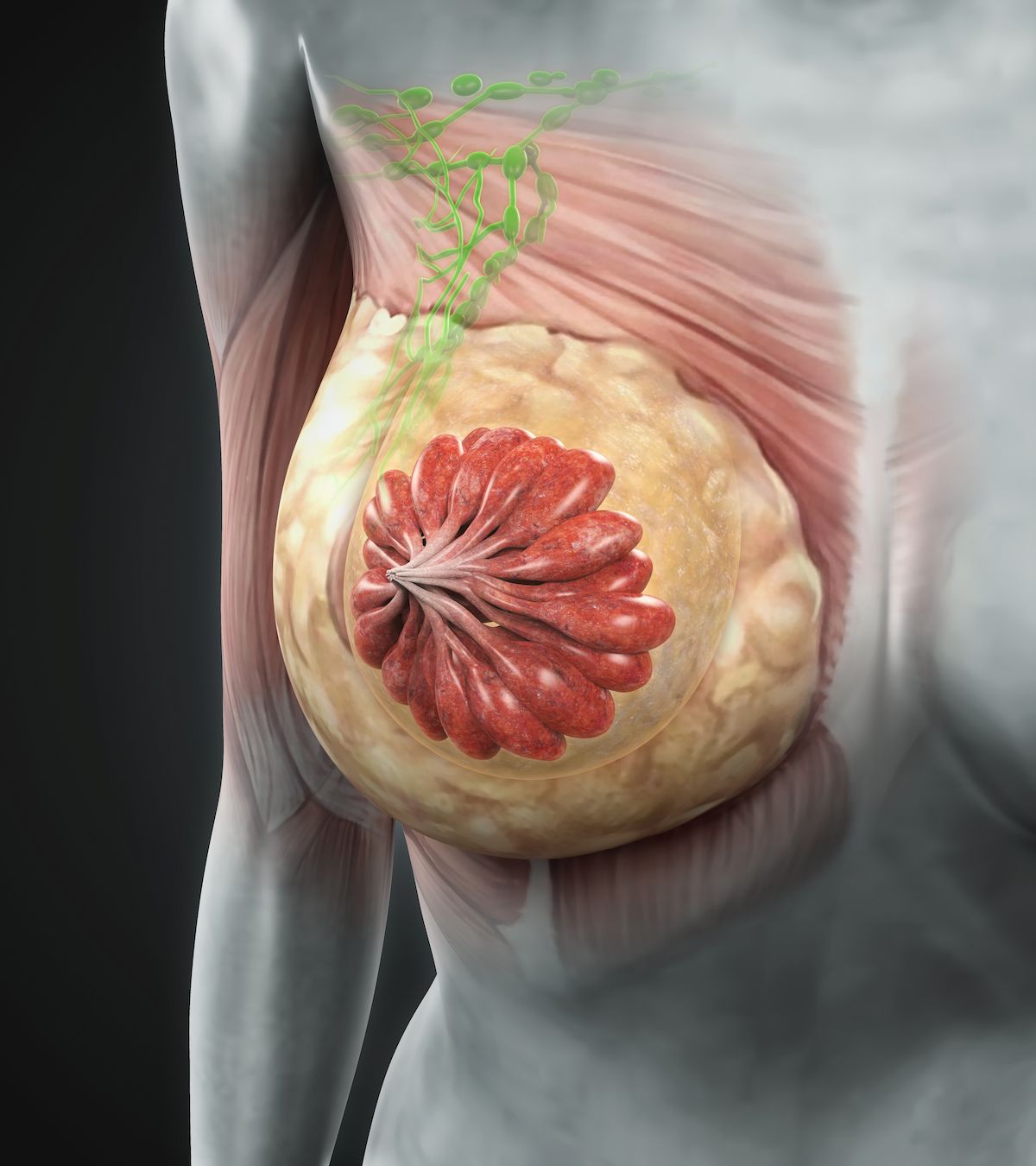
Supplementary imaging between screening mammograms may be underused in patients at high risk for breast cancer, while services may be overused in those with dense breasts without other risk factors, according to findings from a study published in Cancer Medicine.
The analysis assessed incongruent screening, which was defined for patients at average risk as the receipt of supplemental imaging between screening mammograms, and for patients at high risk as a lack of such supplemental imaging.
In sum, 97.7% of patients at high risk were incongruently screened compared with0.9% of those at average risk (P <.01). In the latter group, 2.0% of those with dense breasts were incongruently screened vs 0.1% of those with non-dense breasts (P <.01). Conversely, in the high-risk group, incongruent screening was more likely among those with non-dense (99.5%) vs dense breasts (95.2%; P <.01). There was a weaker association between risk and incongruent screening among patients with dense (simple slope, 3.71; P <.01) vs nondense breasts (simple slope, 5.79; P <.01).
Age and race did not have a significant impact on rates of incongruent screening overall.
“Guidelines indicate that high-risk [patients] should be screened with supplemental MRI in addition to screening mammogram, and the benefits of early detection support supplemental screening for high-risk [patients] outweighs the potential harms of overdiagnoses and false positives,” the investigators wrote. “Our results are consistent with prior studies, which have found underutilization of supplemental screening modalities, particularly MRI, among [patients] who are at high risk for breast cancer, indicating potential underscreening for an at-risk population of [patients].”
Investigators derived these data from a sample of 4462 Black and 1628 White patients who underwent at least 2 screening mammograms at the Karmanos Cancer Institute in Detroit, Michigan, between January 2016 and March 2018.
In total, 86.5% of this population were at average risk for breast cancer, 7.7% were at intermediate risk, and 5.8% were at high risk. Additionally, 23.8% had dense breasts. The mean age at diagnosis was higher among those at average risk for disease (62.1 years) than those at high risk (52.2 years).
Compared with Black patients, White patients were more likely to be at high risk (7.8% vs 5.1%) and intermediate risk (10.7% vs 6.6%) for breast cancer. White patients had a mean age of 62.53 years compared with a mean of 60.51 years among Black patients.
Investigators classified patients in this sample as high risk for breast cancer if their lifetime risk was 20% or greater, as intermediate risk if lifetime risk was between 15% and 20% and average risk if their lifetime risk was under 15%.
The generalizability of these findings are limited by the fact that they derive from a single screening center in a metropolitan academic setting, according to the investigators. Moreover, the study did not account for the sociodemographic characteristics of referring physicians.
“Whereas health organizations promote evidence-based guidelines for supplemental breast cancer screening in service of patient health, the lack of adherence to these guidelines is concerning,” the investigators concluded. “These findings support the need for interventions to support guideline-congruent behavioral decision-making related to supplemental breast cancer screening so that we may ensure that [patients] are more likely to partake in secondary screening measures in line with evidence-based recommendations.”
Reference
Wehbe A, Gonte MR, O'Neill SC, et al. Predictors of nonadherence to breast cancer screening guidelines in a United States urban comprehensive cancer center. Cancer Med. Published online June 17, 2023. doi:10.1002/cam4.6182