Nonpalpable Intratesticular Mass in a Young Man With a History of Contralateral Retractile Testis
A 24-year-old otherwise healthy man with a history of retractile right testicle managed with right orchidopexy at age 9 presented with a several weeks’ history of discomfort in the left testicle. He has no family history of testicular cancer.
Oncology (Williston Park). 31(6):484, 489–491.

Figure 1. Ultrasound of Left Testicle—demonstrating (A) an 8-mm hypoechoic lesion; (B) with presence of Doppler flow.
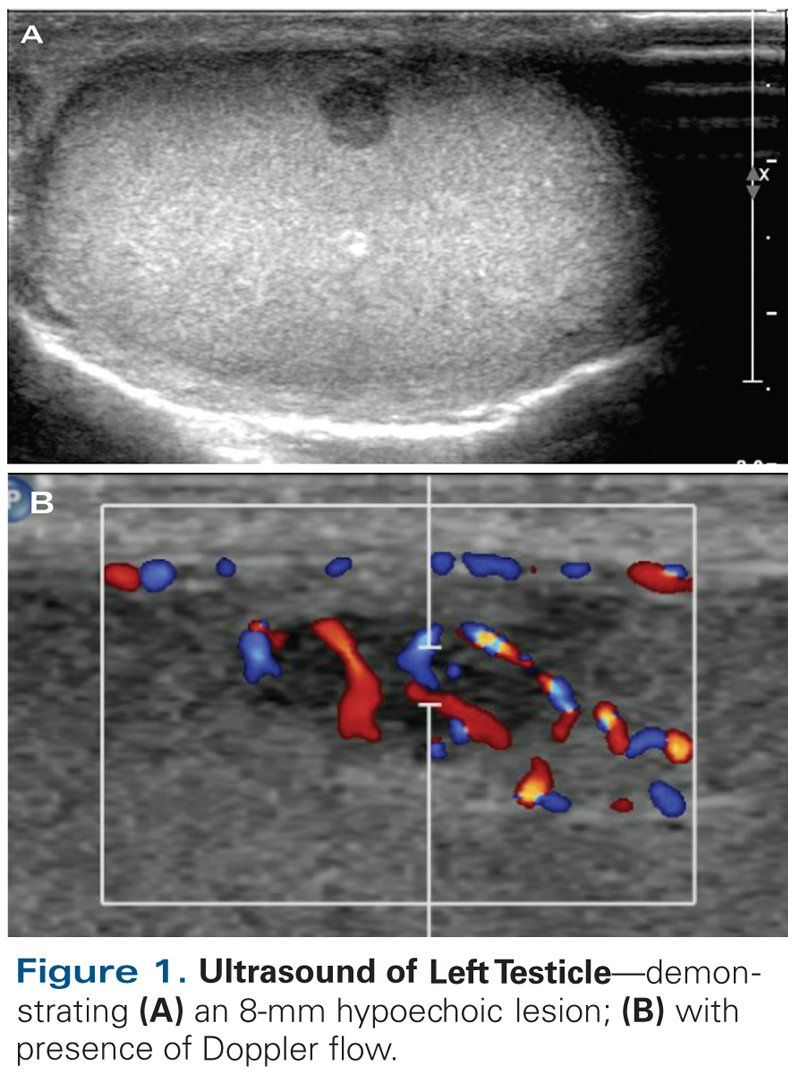
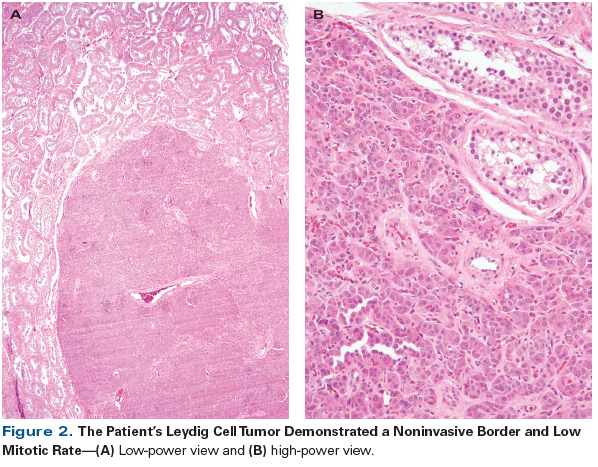
Figure 2. The Patient’s Leydig Cell Tumor Demonstrated a Noninvasive Border and Low Mitotic Rate
The Case
A 24-year-old otherwise healthy man with a history of retractile right testicle managed with right orchidopexy at age 9 presented with a several weeks’ history of discomfort in the left testicle. He has no family history of testicular cancer. Ultrasound revealed a left-sided, 8-mm, hypoechoic intratesticular lesion with increased Doppler flow, consistent with an intratesticular malignancy (Figure 1). Both testicles were equal in size. The left testicle contained multiple calcifications; the right testicle was without lesions. The mass was not palpable on physical examination, and no other intrascrotal pathology was identified. The patient did not have gynecomastia or breast tenderness. Tests for serum tumor markers were negative. An MRI scan of the left testicle, with and without gadolinium, showed the lesion to be 7 mm in size, avidly enhancing, and most consistent with seminoma.
Which of the following represents the best next step in management for this patient?
A. Inguinal radical orchiectomy with preoperative sperm banking
B. Percutaneous, image-guided biopsy of the testis mass
C. Surveillance with high-resolution ultrasound and physical examination
D. Inguinal partial orchiectomy with frozen section examination
Discussion
We present the case of a 24-year-old man with a symptomatic, nonpalpable tumor of the left testicle, with normal serum tumor markers and a history of right orchidopexy for retractile testis-and the resulting treatment decision dilemma. The overall prevalence of testicular cancer is low-1% to 2%-but it represents the most common malignancy in males aged 15 to 45 years.[1] Males who present with a palpable testis tumor harbor a malignant germ cell tumor in > 90% of cases.[2] Thus, radical orchiectomy (Answer A) remains the standard of care for intratesticular tumors.
However, small nonpalpable testis tumors are increasing in prevalence as a result of the widespread use of high-resolution ultrasound. Unlike with palpable tumors, 80% of nonpalpable testicular lesions diagnosed with ultrasound are thought to be benign.[3] Overtreatment of benign testicular lesions may lead to hypogonadism, infertility, and psychological distress.[4] Consequently, alternatives to radical orchiectomy have been proposed.
Percutaneous biopsy could in theory determine, in a minimally invasive manner, whether a lesion was malignant and would thus necessitate radical surgery. However, percutaneous biopsy of testicular tumors (Answer B) is not currently recommended. Scrotal violation has historically been a concern among urologic oncologists, since early studies showed increased recurrence rates, as well as a theoretical risk of disrupted lymphatic spread causing unpredictable patterns of metastatic disease. A recent meta-analysis confirmed an increased risk of local recurrence of 2.9% with scrotal violation, compared with 0.4% without.[5] Interestingly, scrotal violation did not affect survival or distant recurrence rates in this analysis. Published series of percutaneous testis biopsy have not shown evidence of tumor seeding, but the small number of patients undergoing this technique in the literature is unlikely to reverse the current standard of avoiding scrotal violation.[6]
The growing number of small, nonpalpable, benign testis tumors discovered on ultrasound has also led to the adoption of active surveillance as an organ-sparing approach at some centers. A retrospective series of 46 patients with nonpalpable testicular masses incidentally diagnosed on ultrasound during infertility evaluations concluded that active surveillance was safe.[7] All masses were hypoechoic on ultrasound and less than 1 cm in size. Surveillance was typically performed with repeat ultrasound (along with physical examination) at 1, 3, and 6 months. Eight patients eventually underwent surgery, six because of patient preference and two for interval growth on ultrasound. All patients had benign lesions, with the exception of one patient, in whom localized seminoma was diagnosed after 3 mm of growth was demonstrated over 3 months. It should be noted that the mean follow-up in this study was under 1 year, and that it was a retrospective study, with no rigid surveillance protocol in place. Thus, active surveillance (with ultrasound and physical examination) currently represents a significant deviation from the standard of care, and so Answer C is incorrect.
Another alternative approach whose increased use has been advocated in adults with testicular tumors is that of organ-sparing surgery. It should be noted that in prepubertal males, the higher likelihood of a benign tumor has led pediatric urologists to consider partial orchiectomy with intraoperative frozen confirmation as an appropriate approach to nonpalpable testis tumors in children.[8] Testis-sparing surgery in adults, however, is not included in current National Comprehensive Cancer Network guidelines, although the European Germ Cell Cancer Consensus Group and the European Association of Urology guidelines recommend partial orchiectomy with frozen section in very specialized cases,[9-11] including:
•unclear diagnosis
•bilateral tumors
•solitary testicle with normal preoperative serum testosterone levels
These criteria lend support to an argument for partial orchiectomy with frozen section examination in this case, where there is a history of contralateral retractile testis. Although preoperative imaging was suggestive of neoplasm, testicular volume was similar bilaterally, suggesting adequate contralateral gonadal function. MRI has been shown to be a reliable means of determining whether a lesion is benign or malignant (although MRI findings were not consistent with the final pathology in this case).[12] Nonetheless, in the United States, partial orchiectomy with frozen section examination (Answer D) has not been adopted as a standard of care.
The major concern with partial orchiectomy is the potential multifocality of testis cancer. In one series, Ehrlich et al found that 63% of patients with germ cell tumors smaller than 2 cm had additional sites of invasive disease.[13] Thus, the concept of testis sparing in the presence of a normal contralateral testis to avoid orchiectomy for a benign mass is fully reliant on either the ability to accurately determine histology with intraoperative frozen section analysis or a guarantee of adequate oncologic equivalence for salvage treatment, should the excised tumor turn out to be malignant.
Frozen section analysis has been shown to be highly effective at identifying benign and malignant testicular histology. Elert et al correctly identified all malignant and benign lesions on frozen section in 354 patients.[14] Another small series of 15 patients, from Leroy et al, correctly identified all malignant lesions on frozen section but failed to identify all benign lesions, resulting in sensitivities of 100% and 81%, respectively.[15] These results are encouraging, but studies of frozen section outcomes are limited to a few high-volume centers and may not accurately reflect what the results would be in other settings, considering that this is a relatively rare cancer.
In the event of incorrect frozen section analysis, some recommend completion orchiectomy, but there is limited information available on treatment outcomes. Gentile et al describe 1 patient who required orchiectomy for liposarcoma on final pathology after testis-sparing surgery for a suspected benign lesion; he was without recurrence at less than 12 months of follow-up.[16] The German Testicular Cancer Study Group has reported long-term results of 73 patients with either synchronous or metachronous germ cell tumors treated with organ-sparing surgery. Four patients experienced local recurrence between 4 and 165 months postoperatively; all recurrences were successfully treated with completion orchiectomy.[17] After 7 years of follow-up, 98.6% of these patients showed no evidence of disease; however, progression to metastatic disease, requiring adjuvant chemotherapy, occurred in 4.1% within a 2-year period. Additionally, 82% of patients had ipsilateral carcinoma in situ and required adjuvant testicular radiation.[17]
Thus, current urologic texts and guidelines suggest a very limited role for testis sparing. The latest edition of Campbell-Walsh Urology clearly states that there is “no role” for testis-sparing surgery if there is a normal contralateral testicle,[18] and patients such as this young man will most likely continue to be treated with radical orchiectomy.
Outcome of This Case
KEY POINTS
- Small nonpalpable testicular masses < 1.6 cm are benign in up to 80% of cases.
- Frozen section examination is reliable at determining benign and malignant lesions at high- volume centers.
- At present, radical orchiectomy remains the standard of care for testicular masses in the presence of a normal contralateral testis.
Our patient underwent an uneventful left inguinal radical orchiectomy. Pathologic review identified a 7-mm, pT1 Leydig cell tumor (Figure 2). Leydig cell tumors are the most common stromal tumors, accounting for 70% of non–germ cell testis lesions. They are predominantly benign; however, 10% are reported to be malignant, with the retroperitoneum and lungs as the most common sites of metastatic spread. They are resistant to both radiation and chemotherapy and have a very poor prognosis when metastatic. The pathologic criteria for malignant Leydig cell tumors outlined by Kim et al include high mitotic rate, invasive edges, lymphovascular invasion, and nuclear atypia. Clinically, Leydig cell tumors larger than 5 cm are most likely to be malignant.[19]
This case highlights an important dilemma in the current management of nonpalpable testis masses: Should we begin to consider testis sparing in carefully selected adults with smaller lesions and no elevated markers? While it should be clearly stated that the standard of care (particularly in the United States) remains radical orchiectomy when malignancy is suspected, recent and developing data may provide support for a less aggressive approach. Evidence in support of testis sparing is provocative, and results are encouraging. However, the small number of patients reported in the literature should temper enthusiasm for a technique that currently lacks the long-term follow-up data to justify its use in place of radical orchiectomy. Until such data are available, patients should be counselled appropriately that if testis sparing is desired, it is not without risk and outcomes are uncertain.
Financial Disclosure:The authors have no significant financial interest in or other relationship with the manufacturer of any product or provider of any service mentioned in this article.
If you have a case that you feel has particular educational value, illustrating important points in diagnosis or treatment, you may send the concept to Dr. Crawford at david.crawford@ucdenver.edu for consideration for a future installment of Clinical Quandaries.
References:
1. Manecksha RP, Fitzpatrick JM. Epidemiology of testicular cancer. BJU Int. 2009;104:1329-33.
2. La Vecchia C, Bosetti C, Lucchini F, et al. Cancer mortality in Europe, 2000-2004, and an overview of trends since 1995. Ann Oncol. 2010;21:1323-60.
3. Giannarini G, Diekmann K, Albers P, et al. Organ-sparing surgery for adult testicular tumours: a systematic review of the literature. Eur Urol. 2010;57:780-90.
4. Nord C, Bjoro T, Ellingsen D, et al. Gonadal hormones in long-term survivors 10 years after treatment for unilateral testicular cancer. Eur Urol. 2003;44:322-8.
5. Capelouto C, Clark P, Rasil BJ, et al. A review of scrotal violation in testicular cancer: is adjuvant local therapy necessary? J Urol. 1995;139:1225-8.
6. Soh E, Berman LH, Grant JW, et al. Ultrasound-guided core-needle biopsy of the testis for focal indeterminate intratesticular lesions. Eur Radiol. 2008;18:2990-6.
7. Toren PJ, Roberts M, Lecker I, et al. Small incidentally discovered testicular masses in infertile men-is active surveillance the new standard of care? J Urol. 2010;183:1373-7.
8. Ross JH, Kay R. Prepubertal testis tumors. Rev Urol. 2004;6:11-8.
9. National Comprehensive Cancer Network. Testicular cancer. Version 2.2017. https://www.nccn.org/professionals/physician_gls/pdf/testicular.pdf. Accessed April 2, 2017.
10. Albers P, Albrecht W, Algaba F, et al. European Association of Urology guidelines on testicular cancer. Limited update March 2015. https://uroweb.org/wp-content/uploads/11-Testicular-Cancer_LR1.pdf. Accessed April 2, 2017.
11. Krege S, Beyer J, Souchon R, et al. European consensus conference on diagnosis and treatment of germ cell cancer: a report of the second meeting of the European Germ Cell Cancer Consensus group (EGCCCG): part I. Eur Urol. 2008;53:478-96.
12. Tsili AC, Argyropoulou MI, Sofikitis N, Tsampoulas K. MRI in the characterization and local staging of testicular neoplasms. AJR Am J Roentgenol. 2010;194:682-9.
13. Ehrlich Y, Konichezky M, Yossepowitch O, Baniel J. Multifocality in germ cell tumors. J Urol. 2009;181:1114-9.
14. Elert A, Olbert P, Hegele A, et al. Accuracy of frozen section examination of testicular tumors of uncertain origin. Eur Urol. 2002;41:290-3.
15. Leroy X, Rigot JM, Aubert S, et al. Value of frozen section examination for the management of nonpalpable incidental testicular tumors. Eur Urol. 2003;44:458-60.
16. Gentile G, Brunocilla E, Franceschelli A, et al. Can testis-sparing surgery for small testicular masses be considered a valid alternative to radical orchiectomy? A prospective single-center study. Clin Genitourin Cancer. 2013;11:522-6.
17. Heidenreich A, Weissbach L, Holtl W, et al. Organ sparing surgery for malignant germ cell tumor of the testis. J Urol. 2001;166:2161-5.
18. Stephenson AJ, Gilligan TD. Neoplasms of the testis. In: McDougal WS, Wein AJ, Kavoussi LR, et al, editors. Campbell-Walsh urology. 11th ed. Philadelphia: Elsevier; 2015. pp. 784-814.
19. Kim I, Young RH, Scully RE. Leydig cell tumors of the testis: a clinicopathological analysis of 40 cases and review of the literature. Am J Surg Pathol. 1985;9:177-92.