Notch Signaling Important in AML Development
Activating mutations in the beta-catenin gene in bone cells is shown to contribute to the development of acute myeloid leukemia.
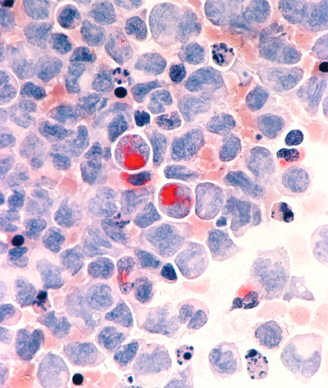
Acute myelocytic leukemia in the pericardial fluid, shown with an esterase stain at 400x
Activating mutations in the beta-catenin gene in bone cells is shown to contribute to the development of acute myeloid leukemia (AML). Part of the Notch signaling pathway important in development and implicated in cancer formation, beta-catenin and other genes in the pathway may be appropriate targets for AML therapies. The study suggests that Notch signaling is required for AML development in mice with activating beta-catenin mutations.
Using mouse models, Stavroula Kousteni, PhD, assistant professor of medicine in the department of pathology and cell biology at Columbia University in New York, and colleagues identified a potential new target for treatment. The study also provides evidence that beta-catenin is activated in the osteoblasts of patients with AML and also myeloproliferative disease, a related hematological disorder, suggesting that a similar mechanism may be important in the development of AML in humans.
The results are published in the journal Nature.
Kousteni and colleagues found that an activating mutation in the beta-catenin of mouse osteoblasts changes the differentiation of myeloid progenitors and is enough to initiate development of AML with common chromosomal mutations.
Genetic changes in osteoblast precursor cells of the bone have been previously shown to affect the dynamics of hematopoietic stem cells, including homing of these stem cells, their mobilization, and B-cell lymphopoiesis. At least in mice, these osteoblast cells have an influence on the development of pre-leukemia cells, but the genetic mutations that can lead to the evolution of this pre-leukemia state was not previously known.
“That a mutation in a cell that does not belong to the hematopoietic lineage not only can influence nearby cancer cells but can transform neighboring healthy hematopoietic stem cells to leukemic ones and induce the appearance of mutations that are reminiscent of the human disease and establish self-propagating AML that can be transferred in healthy recipient is what is novel about this work,” Kousteni told Cancer Network. “The study also clarified the exact mechanism that led to the leukemogenic transformation,” she said.
In the current study, the authors found that mice with the constitutively active beta-catenin allele in osteoblasts (ctnnb1 gene) are anemic by 2 weeks of age and die at 6 weeks of age. Activation of beta-catenin led to activation of the Notch ligand jagged 1 in the osteoblasts and continued Notch pathway signaling led to the malignant changes in the myeloid lineage.
Mutating one jagged 1 allele alleviated the anemia, lowered Notch signaling in the beta-catenin mutant mice, and in contrast to the beta-catenin mutants, resulted in normal mice. Inhibition of Notch signaling with a gamma-secretase inhibitor also reversed the hematopoietic deregulation.
Examining bone marrow biopsies in 107 samples from patients with either myelodysplastic syndromes or AML showed that 38% (41 of 107) of the patients had increased beta-catenin signaling in the osteoclasts and increased Notch pathway signaling in the hematopoietic cells. The authors are now characterizing these patients by age, severity of disease, and other genetic characteristics, said Kousteni.
Kousteni says that targeting the microenvironment where the cancer cells grow may be a potential way to treat the leukemia, targeting the healthy rather than the myeloid blast cells, which are the evolving population of clonally expanding cells.
The authors are now studying how soon after the beta-catenin mutation is expressed in mice that AML is induced and if defects in hematopoiesis during development predispose the mice to AML. “We are also looking into different means of blocking the leukemogenic signal in our mouse model, either by blocking b-catenin signaling or Notch signaling using a combination of small molecules or blocking antibodies,” said Kousteni.
The Leukemia and Lymphoma Society estimate that there are more than 35,000 people in the United States with AML and that more than 14,500 new cases will be diagnosed this year. About 10,370 people died of AML in the United States in 2013. Some progress has been made in AML, in particular with stem cell transplantation that benefits younger patients, but the disease is still incurable and has a poor prognosis. “After 3 decades we are still relying on two drugs-cytarabine and an anthracycline-for therapy,” said Kousteni. “There have not been any new treatments for myelodysplastic syndromes in 30 years. Identifying potential targets that may contribute to these diseases may also impact therapy,” she added.