Novel Approach of Phase I/II Trial Seeks Optimal Rather Than Maximum Tolerated Dose for Potent Epigenetic Drug Targeting Myelodysplastic Syndromes and Leukemia
Preliminary findings of a phase I/II randomized clinical trial indicate that SGI-110, a novel DNA methylation inhibitor, is safe, well tolerated and efficacious in patients with acute myelogenous leukemia.
CHICAGO-Preliminary findings of a phase I/II randomized clinical trial indicate that SGI-110, a novel DNA methylation inhibitor, is safe, well tolerated, and efficacious in patients with acute myelogenous leukemia (AML), reported Jean-Pierre Issa, MD, professor of medicine and director of the Fels Institute for Cancer and Molecular Biology at Temple University, Philadelphia (AACR abstract LB-214). SGI-110 is a second generation hypomethylating agent designed as a dinucleotide of decitabine and guanosine, to prolong in vivo exposure and potentially improve efficacy of decitabine by protecting it from rapid deamination by cytidine deaminase.
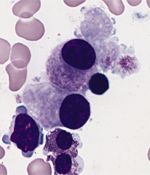
Bone marrow smear from a patient with RAEB and an isolated 5q-chromosome abnormality: megakaryocytes with a nonlobulated nuclei in a myelodysplastic syndrome.
The study, funded by a Stand Up to Cancer research grant, used a novel design to establish a biologically effective and tolerable dose of SGI-110 in patients with either myelodysplastic syndromes or leukemia. This differs from the traditional use of maximum-tolerated dose in phase I trial designs. And, according to Dr. Issa, this approach may have revealed a new, potent epigenetic drug that could safely alter the way cancer cells function within the body.
“I compare it to war and diplomacy,” said Dr. Issa. Traditional cancer drugs declare war on cancer cells by killing them. In contrast, he explained, DNA methylation inhibitors use “diplomacy” to try to alter cancer cells, which is less toxic and debilitating for patients.
The epigenetic code studied can be thought of as small tags that decorate DNA and provide instruction for how the body uses DNA, according to Dr. Issa. In patients with cancer, this code has become abnormal. DNA methylation inhibitors attempt to normalize these tags and the code of cancer cells. “These drugs try to remind the cancer cell of its normal origin and proper behavior,” he said. “They remove these ‘tags’ and rewrite the instruction manual.”
According to Dr. Issa, decitabine currently has limited efficacy because it is quickly degraded in the body. SGI-110 has the potential to demonstrate prolonged drug exposure and improved efficacy through protection from degradation.
In the first in-human study of SGI-110, Dr. Issa and colleagues randomly assigned patients with relapsed or refractory intermediate- or high-risk myelodysplastic syndromes or leukemia to subcutaneous daily injections of SGI-110 for 5 days or to weekly injections for 3 weeks. Results so far indicate that SGI-110 is well tolerated, with local injection site pain, neutropenia, thrombocytopenia, and anemia as observed adverse effects. To date, the investigators have recruited 66 patients.
SGI-110 was also found to have an extended half-life and produce clinical response. At least 2 patients have had disease remission, with 1 complete response and 1 partial response, Dr. Issa reported.
“There have been some remarkable results in patients who have no options left to them,” he noted. A phase II study will soon be under way to further explore SGI-110 doses. In addition, Dr. Issa and colleagues are beginning to design studies exploring the use of the drug in other, more common solid tumors such as lung cancer and breast cancer.
Using Stand Up to Cancer’s grant model of collaborative research, Dr. Issa and colleagues worked with Astex Pharmaceuticals to develop SGI-110.