In NSCLC, Beta-3 Tubulin Isoform Does Not Predict Treatment Response to Ixabepilone, Paclitaxel
Expression of the beta-3 tubulin (ß3T) isoform was a negative prognostic factor in non–small-cell lung cancer (NSCLC) patients, but did not predict treatment response for either paclitaxel or tubulin-inhibiting chemotherapy with ixabepilone.
Expression of the beta-3 tubulin (3T) isoform was a negative prognostic factor in non–small-cell lung cancer (NSCLC) patients, but in a new study, it did not predict treatment response for either paclitaxel or tubulin-inhibiting chemotherapy with ixabepilone. The randomized phase II trial results were published online ahead of print on April 15 in the Journal of Clinical Oncology.
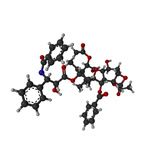
Ball-and-stick model of paclitaxel
Previous research has also suggested a negative prognosis in NSCLC with higher levels of 3T expression, particularly due to an increased rate of metastasis. Ixabepilone is an epothilone, a novel class of agents that bind to and stabilize microtubules. Researchers led by Martin J. Edelman, MD, of the University of Maryland School of Medicine, conducted a trial of ixabepilone along with carboplatin vs paclitaxel and carboplatin, with both groups stratified by 3T status (positive or negative). Of 95 ixabepilone patients, 52 were 3T positive and 43 were 3T negative; of the 96 paclitaxel patients, 49 were 3T positive and 47 were 3T negative.
The median progression-free survival was 4.3 months in the 3T-positive patients in both treatment arms (P = .853); in 3T-negative patients, the median progression-free survival was 5.8 months for ixabepilone and 5.3 months for paclitaxel (P = .350). Progression-free survival for ixabepilone and paclitaxel was also similar across the overall patient population regardless of 3T expression.
Furthermore, overall survival did not differ significantly in the 3T-positive subset of patients, which investigators hypothesized might be the case. The median overall survival for 3T-positive ixabepilone patients was 10.61 months, compared with 11.37 months for paclitaxel patients (P = .053). In only the 3T-negative patients, overall survival was 16.92 months for ixabepilone and 9.40 months for paclitaxel (P = .123). Adverse events were generally mild to moderate in both groups, and were largely similar across treatments.
“I am not surprised that 3T was a negative prognostic factor, this had been seen in many retrospective series,” Dr. Edelman said in an e-mail. “I was disappointed that there was no difference in outcome based upon the 3T expression between the paclitaxel and ixabepilone arms. Based upon a substantial amount of evidence, we believed that we would see a significant difference.” The authors wrote that further trials could still illuminate whether 3T expression can be used to guide therapy, or if it is simply a prognostic marker with no value in terms of treatment modalities.