Number of Moles Not Always Related to Likelihood of Melanoma
The number of moles, or nevi, a patient had was not related to the likelihood that they had melanoma, according to the results of a new study.
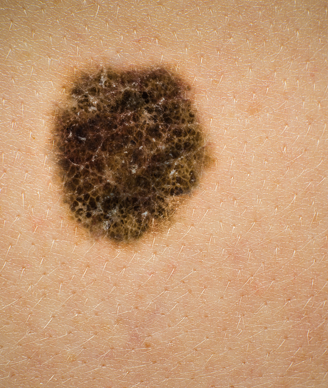
Image © Australis Photography / Shutterstock.com
The number of moles, or nevi, a patient had was not related to the likelihood that they had melanoma, according to the results of a new study published in JAMA Dermatology. In fact, the study found that most patients with melanoma had very few nevi and no atypical nevi.
“Having many total nevi [TN] or any atypical nevi [AN] is often reported to be a major risk factor for melanoma by public advocacy organizations However, it appears from the present large case series that many patients with melanoma do not routinely have an increased mole count or AN,” wrote researcher Alan C. Geller, MPH, RN, of Harvard T.H. Chan School of Public Health, and colleagues.
Based on these results, the researchers wrote that “physicians and patients should not rely on the total nevus count as a sole reason to perform skin examinations or to determine a patient’s at-risk status.”
The study surveyed 566 patients at two academic sites and an affiliated Veterans Affair medical center. Patients were surveyed within 3 months of their melanoma diagnosis. The researchers looked at the TN count and the AN count performed at the patient’s first visit after diagnosis. Patients were then grouped for TN into groups from 0 to 20, 20 to 50, or more than 50 and for AN, groups of 0, 1 to 5, or more than 5. Finally, tumor thickness was categorized at 2.0 mm or less or 2.01 mm or more.
A majority of the patients diagnosed with melanoma had between 0 and 20 TN (66.4%) and no AN (73.3%). About one-fifth of patients had 20 to 50 TN, and 13.1% had more than 50 TN; 14.5% of patients had 1 to 5 AN, and 12.2% had more than 5 AN.
Results showed that the average tumor thickness was 2.33 mm for patients with 0 to 20 TN and 0 AN, but decreased to 1.12 mm for patients with more than 50 TN and 0 AN. The thickest melanomas were found in patients with 20 to 50 TN and at least 1 AN.
“Thinner melanomas in patients with more TN might be due to a less aggressive biological behavior of melanoma and a tendency of these patients to have their moles checked more frequently, whereas having more AN may make discovery by either the patient or his or her physician more difficult because the true ‘outlier’ melanoma may be less easily recognized,” the researchers wrote. “This latter explanation may relate to pattern recognition, such that it is easier for a person with many common nevi to see the ‘ugly duckling’ outlier nevus compared with an individual with many AN, which share clinical features with melanoma but are rarely true melanoma precursors.”
The researchers also looked at the results by patient age and found that in patients younger than 60, having 50 or more TN resulted in an almost 70% reduced risk for having a thick melanoma (odds ratio [OR], 0.32 [95% CI, 0.12–0.81]). In addition, patients aged younger than 60 who had more than 5 AN had more than twice the risk for a thicker melanoma compared with patients with no AN (OR, 2.43 [95% CI, 1.02–5.75]). These associations were not found in patients aged older than 60.
“Our findings raise the question as to whether major public health messages overstate the emphasis on many TN or AN and suggest that at-risk patients and their health care professionals should be equally concerned about melanoma risk in those with few nevi,” the researchers wrote.
2 Commerce Drive
Cranbury, NJ 08512
All rights reserved.