Omitting Lymphadenectomy Reduces AEs, Does Not Lower DFS in Cervical Cancer
The 3-year DFS rate was 96.9% in patients who received sentinel-lymph node biopsy alone vs 94.6% in those who received lymphadenectomy.
The 3-year DFS rate was 96.9% in patients who received sentinel-lymph node biopsy alone vs 94.6% in those who received lymphadenectomy.
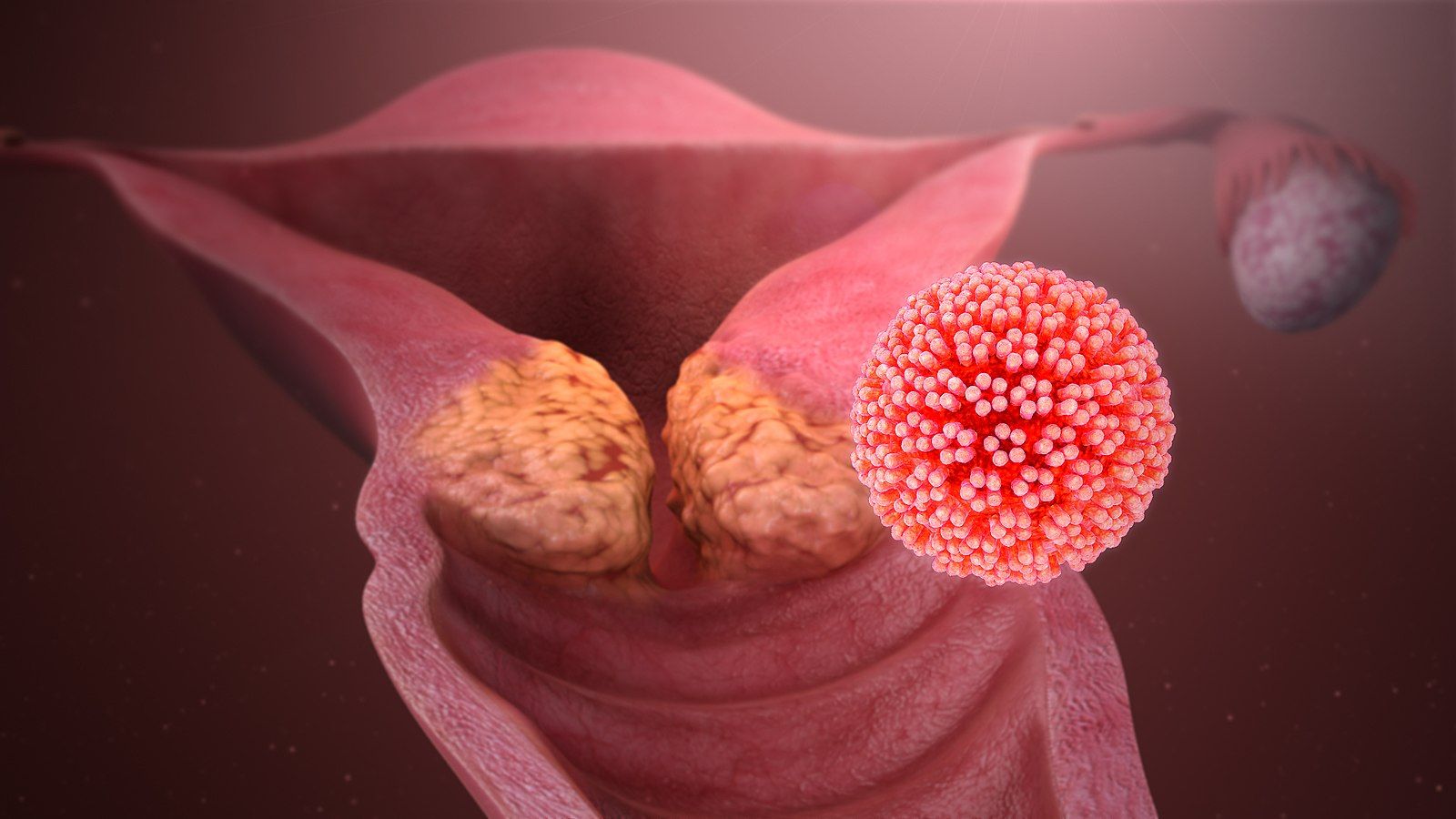
Sentinel-lymph node biopsy alone did not demonstrate notable declines in disease-free survival (DFS) compared with lymphadenectomy while also resulting in fewer toxicities in patients with cervical cancer, according to results from the randomized, noninferiority PHENIX trial (NCT02642471) published in The New England Journal of Medicine.
With a median follow-up of 62.8 months (range, 8.9-110.1), the 3-year DFS rate was 94.6% (95% CI, 91.9%-96.4%) in patients who received lymphadenectomy compared with 96.9% (95% CI, 94.7%-98.2%) in the biopsy-only group (HR, 0.61; 95% CI, 0.33-1.14). The difference between the treatment groups was –2.3 percentage points (95% CI, –5.0 to 0.5). The biopsy-only treatment was found to be noninferior, as the prespecified noninferiority margin in the upper limit of the confidence interval of the between-treatment difference of 5 percentage points was not met.
In the lymphadenectomy group, retroperitoneal nodal recurrences were observed in 2.2% of patients, with 3 having a recurrence in the pelvic nodes, 1 in the paraaortic nodes, and 5 in both; no such recurrences were observed in the biopsy-only group. Furthermore, 2.4% of the lymphadenectomy group had multi-site recurrences, and all recurrences in the biopsy group were in a single site.
The 3-year cancer-specific survival rate was 97.8% in the lymphadenectomy group vs 99.2% in the biopsy alone group (HR, 0.37; 95% CI, 0.15-0.95); in each respective group, 16 and 6 cervical cancer-related deaths occurred.
Subgroup and sensitivity analyses also consistently supported the noninferiority of biopsy-only treatment vs lymphadenectomy. In patients without any protocol violations or deviations, the 3-year DFS rate was 95.5% with lymphadenectomy vs 98.8% with biopsy only (HR, 0.33; 95% CI, 0.13-0.81).
Lymphadenectomy resulted in a median of 27 lymph nodes with both open and laparoscopic surgical approaches. The 3-year DFS rate for patients who underwent laparoscopic surgery was 93.6% (95% CI, 89.8%-96.0%) vs 97.3% (95% CI, 94.5%-98.7%) in the lymphadenectomy vs biopsy-only groups (HR, 0.40; 95% CI, 0.18-0.92). The same improvement was not observed when factoring in patients who underwent open surgery, as the rates were 96.3% (95% CI, 91.1%-98.3%) with lymphadenectomy vs 96.1% (95% CI, 91.6%-98.2%) with biopsy (HR, 1.25; 95% CI, 0.45-3.44).
“Despite its century-long application, pelvic lymphadenectomy has inherent limitations. It prolongs operative duration and carries risks, including vascular and neural injury, lymphedema, lymphocyst, venous thromboembolism, and surgery-related death,” wrote first study author Hua Tu, MD, from the Department of Gynecologic Oncology, Sun Yat-sen University Cancer Center, the State Key Laboratory of Oncology in South China, Collaborative Innovation Center for Cancer Medicine in Guangzhou, China, with coauthors in the publication. “In this trial, sentinel-lymph-node biopsy was noninferior to lymphadenectomy with respect to [DFS] in patients with cervical cancer and was associated with fewer adverse events [AEs].”
A total of 838 patients with cervical cancer were enrolled in the PHENIX-I or node-negative cohort of the PHENIX trial, of whom 420 were in the sentinel-lymph node biopsy group and 418 were in the lymphadenectomy group.
Eligible patients were between 18 and 65 years old with histologically confirmed squamous-cell carcinoma, adenocarcinoma, or adenosquamous carcinoma classified as stage IA1, IA2, IB1, or IIA1 per FIGO 2009 criteria. They also had a tumor diameter of 3 cm or less, absence of radiologic evidence of lymph-node or distant metastasis, an ECOG performance status of 0 or 1, and no desire for fertility preservation.
All patients received sentinel-lymph node mapping at the time of surgery without restrictions on tracers or surgical approaches, and patients without sentinel lymph nodes detected or with obviously metastatic nodes were excluded at screening. Patients either omitted lymphadenectomy in the biopsy-only group or underwent bilateral pelvic lymphadenectomy in the lymphadenectomy group; however, all patients underwent radical hysterectomy, except for patients with stage IA1 cancer, who received simple hysterectomy.
The primary end point of the trial was the 3-year DFS rate. Secondary end points included retroperitoneal nodal recurrence, cancer-specific survival, surgical outcomes, and AEs.
Regarding safety, postoperative AEs occurred in 58.1% of the sentinel-lymph node biopsy group compared with 71.3% of the lymphadenectomy group (P <.001). Significant differences were observed for lymphocyst (8.3% vs 22.0%, respectively; P <.001), lymphedema (5.2% vs 19.1%; P <.001), hypoalbuminemia (6.4% vs 12.9%; P = .001), paresthesia (4.0% vs 8.4%; P = .009), and pain (2.6% vs 7.9%; P = .001). Notably, in the biopsy-only group, lymphedema occurred in more patients who received side-specific lymphadenectomy (15.6%) vs those who did not (3.4%; P <.001); the same was true for lymphocyst, with rates of 15.6% vs 7.0% (P = .02).
“Further investigation may be needed to understand the potential associations of complete lymphadenectomy with retroperitoneal recurrence and cancer-specific mortality,” the authors concluded.
Reference
Tu H, Huang H, Li Y, et al. Sentinel-lymph-node biopsy alone or with lymphadenectomy in cervical cancer. N Engl J Med. 2025;393(15):1463-1474. doi:10.1056/NEJMoa2506267